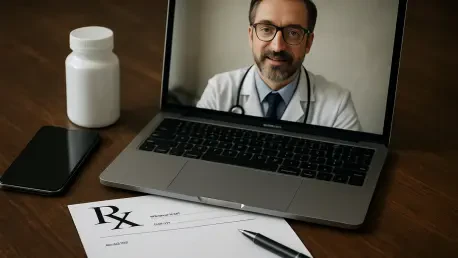
In a significant development for digital healthcare, the Drug Enforcement Administration has once again extended the pandemic-era telehealth flexibilities that permit the remote prescription of controlled substances without a prior in-person medical evaluation. This fourth extension pushes the policy’s expiration to the end of 2026, providing a continued lifeline for millions of patients who rely on virtual consultations for critical medications. The decision came just before the previous deadline, alleviating widespread concern among patients and healthcare providers about a potential “telehealth cliff” that could have abruptly severed access to necessary treatments. The DEA cited two primary motivations for this decision: first, to prevent a sudden and disruptive gap in care for patients currently receiving treatment under these rules, and second, to afford the agency the necessary time to meticulously review the vast number of public comments and finalize a comprehensive set of permanent regulations to govern the practice moving forward. This extension is intended to serve as a bridge, ensuring continuity of care while the final regulatory framework is established.
Navigating the Regulatory Landscape
The announcement was met with a collective sigh of relief from telehealth advocacy organizations, which have been campaigning for the preservation of these vital services. Groups such as ATA Action and the Alliance for Connected Care lauded the DEA’s decision, highlighting its immediate positive impact on countless Americans managing conditions like mental health disorders, substance use disorder, and various chronic illnesses. These flexibilities have been instrumental in breaking down barriers to care, particularly for individuals in rural areas, those with mobility issues, or patients facing other obstacles to in-person visits. However, this praise was tempered with a strong and unified call for a more definitive solution. The pattern of repeated short-term extensions, while beneficial in the immediate sense, has fostered an environment of uncertainty for both clinicians and the patients they serve. This instability complicates long-term care planning and creates a recurring cycle of anxiety as each expiration date approaches, underscoring the pressing need for a stable and predictable regulatory future.
While the extension provides temporary stability, the central focus of the conversation has now shifted to the development of a permanent, forward-thinking policy. Advocacy groups are urging the DEA to collaborate closely with healthcare stakeholders to craft rules that balance patient access with robust safeguards against the potential misuse and diversion of controlled substances. A leading proposal, endorsed by organizations like ATA Action, involves creating a special registration process within the DEA. This framework would allow qualified clinicians who meet specific criteria to register for the express purpose of prescribing controlled medications through virtual means. Such a system would formalize the practice, moving it beyond an emergency measure into a fully integrated and regulated component of modern healthcare. Proponents argue that this approach would maintain the expanded access that has proven so beneficial while implementing the necessary oversight to ensure patient safety and public health, creating a durable solution for the post-pandemic era.
The Path Forward
The extension was a crucial step that prevented an imminent care crisis, but it also underscored the urgency of establishing a permanent regulatory structure. The temporary nature of the current rules has created significant operational and emotional strain for both healthcare systems and patients who depend on consistent access to their medications. This period has demonstrated the immense value and potential of telehealth in delivering essential medical services, particularly for vulnerable populations. The feedback and data gathered during these years of flexible prescribing provide a real-world evidence base that lawmakers and regulators can now use to inform a more lasting policy. This final extension is seen not just as a delay but as a commitment from the DEA to thoughtfully engage with the complexities of virtual medicine and transition from a reactive, crisis-response posture to a proactive, strategic approach for integrating telehealth into the standard of care for the long term.