The journey of a biological specimen from a patient in an operating room to a pathologist’s microscope is one of the most critical and high-stakes processes in modern medicine, yet it has remained alarmingly vulnerable to human error. A recent in-depth analysis of a pilot quasi-experimental study reveals the significant and transformative potential of a specialized Surgical Specimen Chain Management Information System in addressing this long-standing challenge. The research, conducted by Zhang et al., provides compelling evidence that integrating a dedicated information system can substantially mitigate common risks such as specimen misidentification, processing delays, and other handling errors that can have devastating consequences for patient outcomes. This exploration into a technological solution for a persistent logistical vulnerability offers a promising blueprint for healthcare institutions aiming to optimize surgical safety, enhance workflow efficiency, and ultimately elevate the standard of patient care.
The High Stakes of Manual Specimen Handling
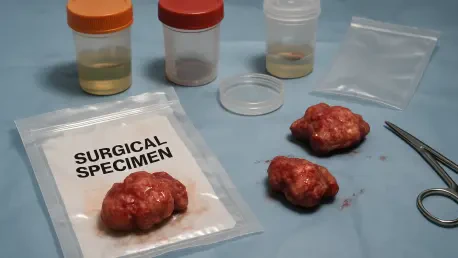
The core problem addressed by the research stems from the inherent complexity and high-pressure nature of the surgical environment, where traditional, often manual, methods for handling specimens are fraught with potential for catastrophic mistakes. Within this fast-paced setting, issues such as mislabeling, accidental specimen loss, or delays in transport to the pathology lab can lead to incorrect diagnoses, the need for unnecessary secondary procedures, or delays in life-saving treatments. Recognizing these systemic vulnerabilities, the researchers designed their study to rigorously evaluate whether a technologically advanced system could create a more secure and efficient “chain of custody” for these vital biological samples. The overarching theme is the crucial transition from fallible, human-dependent processes to a robust, technology-driven framework that ensures absolute integrity and accountability from the moment a specimen is collected until it has been definitively analyzed by a pathologist, closing a dangerous gap in patient safety.
To measure the system’s impact with scientific rigor, the researchers employed a quasi-experimental study design, which allowed for a direct and powerful comparison of specimen management practices before and after the implementation of the new information system. This pre-test/post-test approach was methodically conducted across a diverse range of surgical departments, a strategic choice that significantly strengthens the generalizability of the findings across various complex surgical disciplines. Data collection was meticulously comprehensive, utilizing a mixed-methods approach that combined hard quantitative metrics with insightful qualitative feedback from frontline staff. Key performance indicators that were tracked included the accuracy of specimen identification, the total time elapsed from collection to laboratory processing, and the subjective experiences of the surgical teams. This holistic evaluation provided a deeply nuanced understanding of the system’s impact, capturing not only improvements in objective data but also its profound effect on team coordination and workplace safety culture.
Forging an Unbroken Digital Chain of Custody
The central findings of the study were overwhelmingly positive, indicating a marked improvement in every measured aspect of specimen management following the system’s implementation across all participating departments. This remarkable success is largely attributed to the system’s core functionalities, which are meticulously designed to establish an unbroken and completely transparent chain of custody. A standout feature is the system’s ability to meticulously track each specimen through every stage of its journey. Upon collection in the operating room, each specimen is immediately assigned a unique identifier, typically through a barcode or an RFID tag. This identifier is then inextricably linked to a comprehensive digital record that contains all pertinent information, such as patient details, the precise anatomical origin of the specimen, the exact date and time of collection, and the names of the surgical team members involved. This process of immediate digital documentation virtually eliminates the risks of manual labeling errors and provides a clear, indisputable audit trail, which is crucial for both quality control and ultimate accountability.
Furthermore, the system’s advanced architecture facilitates real-time status updates and instant, secure access to information for all authorized personnel involved in the patient’s care pathway. This dynamic and continuous flow of data allows surgical teams, pathology staff, and other stakeholders to monitor the precise status and location of a specimen at any given moment. Such immediate access supports swift and highly informed decision-making, a capability that is particularly valuable in time-sensitive scenarios such as intraoperative frozen section analysis, where a rapid diagnosis can fundamentally alter the course of the surgical procedure in real time. This enhanced agility not only streamlines the operational workflow within the busy operating room but also fosters a more coordinated and safety-conscious environment, ensuring that all team members are consistently operating with the most current and accurate information available, thereby reducing uncertainty and minimizing the potential for error.
The Human and Clinical Impact of Implementation
The research also underscored a critical success factor that extends far beyond the technology itself: the absolute necessity of comprehensive training and genuine staff engagement. The study emphasized that the full benefits of such an advanced system can only be realized if the end-users—the nurses, surgeons, and technicians on the front lines—are both proficient and comfortable with its daily operation. Consequently, the implementation protocol included the development and delivery of targeted training programs specifically designed to equip surgical teams with the requisite skills and knowledge. By actively involving the staff in the transition process and systematically addressing their concerns, the project cultivated a powerful sense of ownership and facilitated a smoother, more effective adoption of the new technology. This highlights a universal truth in healthcare innovation: successful digital transformation is as much about empowering people as it is about implementing powerful new platforms and software.
The positive impact of the Surgical Specimen Chain Management Information System was shown to extend far beyond the logistical confines of the operating room, creating a ripple effect that touched every aspect of the diagnostic process. The accuracy and timeliness of specimen processing are foundational to the quality of subsequent laboratory analysis. By ensuring that specimens arrived at the pathology lab correctly identified and in optimal condition, the system directly contributed to the accuracy and speed of diagnosis. This, in turn, allowed clinicians to formulate and commence appropriate patient treatment plans more rapidly, which potentially led to significantly improved clinical outcomes and a better overall patient experience. This demonstrated a powerful dual benefit: the system simultaneously enhanced internal operational efficiency for the hospital while elevating the standard of patient safety and care, making it a pivotal advancement in surgical practice.