Unpacking a Critical Moment for Hospital Finances
In 2025, the American healthcare sector stands on the edge of a financial precipice as Congressional funding deadlines threaten the operational stability of hospitals nationwide, creating a dire situation for many facilities. With key payment programs and regulatory flexibilities expiring, the industry faces a staggering risk of closures, reduced care access, and increased uncompensated care costs. Consider this sobering reality: rural hospitals, already operating on thin margins, could shutter without critical payment adjustments, leaving entire communities without local medical services. This market analysis delves into the intricate dynamics of hospital funding, examining current trends, data-driven projections, and the broader implications for healthcare delivery. The purpose is to provide stakeholders with a clear understanding of the challenges and potential pathways forward in a landscape defined by uncertainty and urgent need.
Deep Dive into Market Trends and Financial Pressures
Rural Hospital Vulnerability: Payment Adjustments on the Brink
The expiration of payment programs like the Low-Volume Adjustment (LVA) and Medicare-Dependent Hospital (MDH) represents a significant threat to rural hospitals in 2025. These adjustments, crucial for facilities with limited patient volumes, have historically been extended on a temporary basis, creating a persistent state of financial unpredictability. Data from industry associations indicates that without these funds, a substantial number of rural providers could face closure, disrupting healthcare access for millions in remote areas. The market impact extends beyond individual hospitals, potentially triggering a domino effect of reduced local employment and economic activity in already struggling regions.
Moreover, the lack of long-term funding solutions hampers strategic planning for these facilities. Hospital administrators are forced to operate under the constant shadow of potential budget shortfalls, limiting investments in staff, equipment, and infrastructure. This trend of short-term fixes, while offering momentary relief, underscores a broader market failure to address structural inefficiencies in rural healthcare delivery, pushing the sector toward a critical tipping point.
Medicaid Reductions: A Growing Financial Strain
Another pressing concern in the hospital market is the substantial cut to the Medicaid Disproportionate Share Hospital (DSH) program, which compensates facilities for treating low-income and uninsured patients. With an $8 billion reduction already in effect and further cuts looming, safety-net hospitals are grappling with heightened financial pressures. This reduction coincides with a market environment where coverage expansions have not fully offset the rising costs of uncompensated care, leaving many providers exposed to significant revenue losses.
Projections from analytical bodies suggest that the uninsured population could grow in the coming years, exacerbating the burden on hospitals. As premiums rise and coverage gaps widen, the market may see an uptick in emergency room visits by uninsured patients, further straining hospital resources. This trend highlights a critical mismatch between policy expectations and on-the-ground realities, forcing providers to navigate a shrinking safety net with limited federal support.
Regulatory Rollbacks: Stifling Care Delivery Innovation
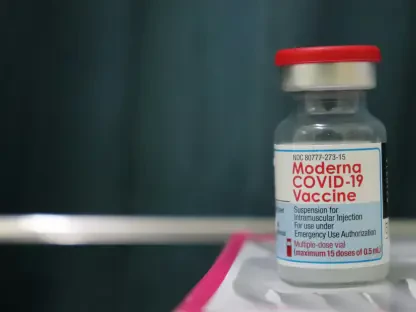
The hospital market is also contending with the expiration of regulatory waivers that have supported innovative care models like telehealth and hospital-at-home programs. These flexibilities, expanded during past health emergencies, have allowed providers to deliver acute care outside traditional settings, reducing costs and improving patient outcomes. Their lapse in 2025 risks reversing these gains, particularly in underserved areas where access to in-person care remains a challenge.
Industry data points to significant benefits from these programs, including enhanced patient satisfaction and lower overhead expenses. However, regional disparities in digital infrastructure pose a barrier to equitable adoption, with rural areas often lacking the broadband necessary for effective telehealth services. This market trend reveals a dual challenge: preserving innovation while addressing inequities, a balance that policymakers must strike to prevent a regression in care delivery standards.
Coverage Losses: The Ripple Effect of Expiring Tax Credits
A longer-term market concern is the impact of expiring enhanced premium tax credits, which have bolstered health insurance affordability for millions. Without an extension beyond the current framework, projections indicate a potential increase of over 4 million uninsured Americans by the end of this decade, alongside premium hikes that could strain household budgets. Hospitals, in turn, face a heightened risk of uncompensated care costs, which could destabilize their financial models.
This trend signals a broader market shift toward increased volatility in insurance coverage, with direct implications for hospital revenue streams. Urban safety-net facilities, in particular, may bear the brunt of this change, as they serve populations most likely to lose coverage. The resulting financial squeeze could accelerate consolidation trends, with smaller hospitals merging into larger systems to weather the storm, reshaping the competitive landscape of healthcare delivery.
Forecasting the Future: Emerging Patterns and Predictions
Looking ahead, the hospital market is poised for significant transformation driven by both policy decisions and economic realities. Bipartisan legislative efforts to delay coverage-related expirations suggest a growing acknowledgment of the crisis, though comprehensive solutions remain elusive. If temporary extensions continue to dominate Congressional responses, the market may see persistent uncertainty, discouraging long-term investments in healthcare infrastructure and innovation.
Technologically, the push for permanent telehealth frameworks could redefine care delivery, potentially lowering costs if supported by robust digital investments. However, without targeted funding to bridge connectivity gaps, this trend risks widening disparities between urban and rural markets. Economically, hospitals may need to explore alternative revenue models, such as partnerships with private payers or state-level programs, to offset federal funding shortfalls.
From 2025 to 2027, projections indicate a potential wave of hospital closures if current funding challenges persist, particularly in rural areas. Industry analyses suggest that mergers and acquisitions could rise as a survival strategy, though this may reduce competition and raise concerns about care quality and pricing. These emerging patterns underscore the urgency of moving beyond stopgap measures toward sustainable policy frameworks that stabilize the market for the long haul.
Reflecting on the Path Forward: Strategic Insights and Actions
Looking back on this analysis, it becomes evident that the hospital sector grapples with a complex web of financial and regulatory challenges in 2025, driven by expiring payment programs, Medicaid cuts, and coverage losses. The market trends point to a fragile ecosystem where rural providers face existential risks, safety-net hospitals absorb growing uncompensated care costs, and innovation in care delivery hangs in the balance. These findings illuminate the profound implications for healthcare access and economic stability across diverse communities.
Moving forward, strategic action is deemed essential to navigate this crisis. Hospitals are encouraged to strengthen advocacy efforts through coalitions, pushing for multi-year or permanent funding solutions while diversifying revenue through private partnerships. Policymakers, on the other hand, need to prioritize data-driven reforms that balance fiscal responsibility with public health imperatives, ensuring that programs like telehealth receive the infrastructure support necessary for equitable impact. For local leaders, building contingency plans and engaging state-level resources offer a buffer against federal delays. Ultimately, collaboration across sectors emerges as the cornerstone for securing a resilient healthcare market, paving the way for innovative solutions and sustained access to care in the years that follow.