With a deep expertise in medical robotics and the Internet of Things, James Maitland is at the forefront of leveraging technology to solve some of healthcare’s most persistent challenges. His work focuses on creating seamless connections between at-home diagnostics and ongoing clinical care, a mission that has culminated in an innovative new partnership with Amazon One Medical. This collaboration aims to redefine preventive health, particularly for those in remote and underserved communities.
In our conversation, we explore the intricate details of this venture. We’ll touch on the logistical hurdles of delivering healthcare to rural America, the user’s journey with a multi-device screening kit, and the critical moment when data turns into a diagnosis. We will also delve into the unique business model that makes this technology both affordable and scalable, and examine the key factors driving its remarkable user satisfaction and engagement.
Your new partnership with Amazon One Medical aims to close care gaps, particularly in rural areas. Could you walk me through the specific logistical and clinical challenges you’re solving for these patients, and how the optional One Medical membership provides them with crucial flexibility?
Absolutely. The challenges for people in rural areas are immense and often invisible to those in cities. We had a powerful story from a family member in rural Oregon that really crystallized this. He needed a simple annual wellness check, but the nearest lab was 80 miles away. He took a day off work, drove all the way there, filled out paperwork, and was then wheeled a computer for a virtual consultation. He was furious, exclaiming how he had just blown an entire day for something that could have been done from his living room. We’re solving that exact problem. By shipping a comprehensive kit anywhere UPS can deliver, we eliminate the travel, the time off, and the frustration. The optional One Medical membership is key to our philosophy; it provides a seamless, high-quality next step for those who need a primary care provider, without forcing anyone to leave a doctor they already trust. It’s about creating access and options, not mandates.
The at-home screening kit integrates multiple FDA-cleared devices for a process that takes 30 to 60 minutes. Can you describe the user’s journey from unboxing the kit to receiving instant results in the app, and what were the key technical hurdles in unifying these different devices?
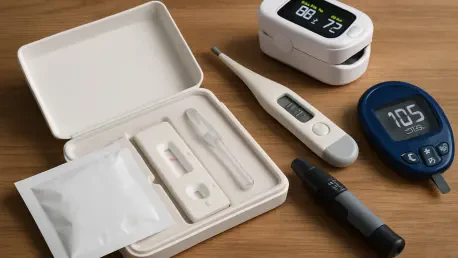
The user journey is designed to be incredibly simple and empowering. You receive a single, consolidated kit at your home. Inside, you find several Bluetooth-connected, FDA-cleared devices—a blood pressure cuff, a scale for BMI, a glucometer, and a device for a full lipid panel. The magic isn’t in creating new hardware, but in our software platform. Our mobile app guides you through each measurement, step-by-step, in a process that takes less than an hour. As soon as a reading is taken, it appears instantly in the app. The biggest technical hurdle was getting devices from different manufacturers, each with its own data protocol, to speak the same language and feed into one unified, intuitive user interface. That’s our secret sauce: creating a seamless digital experience that makes complex health data immediately accessible and easy to understand.
With about half of users discovering a previously unknown health issue, the “handoff” to care is critical. Could you share an anonymized example of this process? What specific steps do a user and the virtual clinician take after an abnormal lipid panel or high blood pressure result?
That’s the most important part of what we do; the data is meaningless without a clear path to action. When we see that about half of our users uncover an issue they weren’t aware of, that handoff becomes our central mission. Imagine a user, let’s call her Sarah, completes her screening and sees her cholesterol and blood pressure are elevated. Her heart sinks a little, but the app immediately prompts her to schedule a virtual visit. Within hours, she’s speaking with a clinician through our ReperioCare service. The clinician already has her results, reviews them in the context of her medical history, and can explain what they mean in simple terms. They might discuss lifestyle changes and, if necessary, prescribe medication. From there, Sarah has a choice: she can take this information to her own doctor or, if she doesn’t have one, we can seamlessly connect her to a primary care physician through the One Medical membership to manage her condition long-term.
Instead of selling devices, you loan, sterilize, and reuse them. How does this model create the 4x to 8x cost savings you’ve measured for employers, and what are the logistical steps involved in managing this reverse supply chain to ensure safety and efficiency?
This model is a complete departure from the consumer-first approach of selling individual devices, and it’s the engine behind our cost-effectiveness. A full suite of these medical devices could cost an individual hundreds of dollars. By loaning the kit, we remove that barrier entirely. An employer pays for the service, not the hardware. When the employee is done, a pickup is scheduled, and the kit is returned to our facility. There, it undergoes a rigorous, multi-step sterilization process to ensure it’s clinically pristine for the next user. This reverse logistics chain is complex, but it allows us to achieve those significant 4x to 8x cost savings for clients. The savings are measured by the value of detecting a serious health concern early, preventing costly emergency room visits or long-term complications down the road.
You’ve achieved a 95% satisfaction rate and boosted screening participation by over 200% for clients. What specific elements of the at-home screening and virtual consultation process do you believe are most responsible for driving this high level of engagement and satisfaction among employees?
The convenience is undeniably the biggest driver. We are meeting people exactly where they are—in their own homes, on their own schedules. Removing the need to travel, take time off work, and sit in a waiting room eliminates the biggest barriers to preventive care. That convenience is what drives the 200% increase in participation. The high satisfaction rate, however, comes from the feeling of empowerment. Users aren’t just getting a lab report a week later; they see their results instantly on their phone. This immediacy makes the connection between their actions and their health tangible. When you pair that with an on-demand virtual consultation to immediately discuss those results, you transform a potentially anxious experience into a proactive, supportive, and deeply personal health journey.
What is your forecast for the at-home preventive care industry over the next five years?
I believe we are at a tipping point. The future of preventive care is decentralized and deeply personalized. My vision is that within five years, any American, no matter how remote their location, will be able to have a full screening kit delivered to their door within an hour. They’ll be able to perform their annual wellness check from their kitchen table, have an immediate virtual consultation to interpret the results, and get any necessary prescriptions delivered straight to their home that same day. The technology is already here. The next five years will be about refining the logistics, expanding payer integration, and making this level of seamless, proactive healthcare the expected standard, not the exception.