Artificial intelligence (AI) is swiftly changing how we diagnose and treat neurological disorders, creating exciting possibilities in medicine. By leveraging advanced technologies, AI enhances accuracy, speeds up diagnostic processes, and reduces costs. This transformation is crucial for managing conditions like Alzheimer’s, Parkinson’s, and multiple sclerosis, which impact millions worldwide. As these technologies become more integrated into healthcare systems, the promise of substantial improvements in patient outcomes becomes increasingly achievable.
The Role of AI in Diagnostics
Advanced Brain Imaging
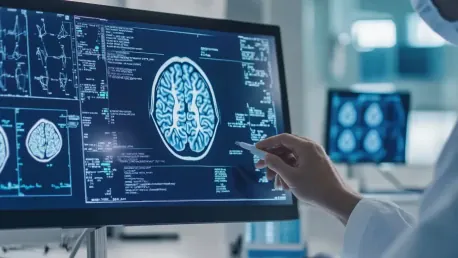
AI’s integration into diagnostics employs machine learning models to analyze vast datasets from brain imaging technologies like MRI and PET scans. These sophisticated tools can detect subtle patterns and anomalies in neuroimaging data that are often missed by human clinicians, providing a significant advantage in diagnosing neurological conditions. For example, in Alzheimer’s disease, AI can identify early signs through alterations in brain structure and function, long before clinical symptoms become apparent. This early detection is vital for effective intervention and managing the disease’s progression.
In the case of Parkinson’s disease, AI algorithms can analyze brain images to monitor changes in motor signs, offering insights into disease evolution and treatment impact. By continuously assessing patient data, AI helps healthcare providers make more informed decisions and tailor treatment strategies accordingly. The sheer volume of neuroimaging data generated through these technologies would be impossible for human specialists to interpret fully, but AI’s capabilities allow for a more comprehensive understanding of complex neurological disorders. This not only improves diagnostic accuracy but also enhances the ability to track disease progression over time.
Predictive Modeling
AI excels in predictive modeling by analyzing rich datasets that incorporate genetic, lifestyle, and environmental data. These models provide a comprehensive risk assessment for developing neurological disorders, enabling timely and preventive measures. For instance, AI can predict the likelihood of an individual developing Alzheimer’s based on biomarkers, cognitive tests, and behavioral factors. This predictive capability allows for earlier interventions, which can potentially delay or prevent the onset of the disease altogether.
The use of predictive modeling extends beyond just risk assessment; it also supports the identification of disease patterns that might be overlooked by human clinicians. By examining vast and varied data sources, AI can reveal intricate connections and trends that inform more precise diagnostic criteria and therapeutic approaches. This holistic view of patient data ensures a more accurate assessment of health risks and helps in creating personalized prevention plans. As a result, individuals at high risk for neurological disorders can receive tailored advice and interventions, ultimately improving their overall health outcomes.
Enhancing Treatment Protocols
Personalized Medicine
The advent of AI in personalized medicine is revolutionizing how treatments are designed and administered for neurological conditions. By analyzing extensive patient data regarding responses to various treatments, AI can recommend personalized therapies tailored to individual needs. This level of customization is crucial for conditions like epilepsy and multiple sclerosis, where treatment efficacy varies significantly from person to person. AI-driven analysis enables clinicians to determine the optimal dosage and combination of medications, adjusting them as necessary to achieve the best possible outcomes.
Personalized medicine through AI also takes into account genetic, environmental, and lifestyle factors, providing a comprehensive approach to treatment. This method ensures that therapies are not only effective but also align with the patient’s unique biological makeup and health history. By continuously monitoring patient responses and outcomes, AI systems can adapt treatment plans in real-time, ensuring timely adjustments that enhance therapeutic efficacy. Patients benefit from more targeted and efficient interventions, which can lead to improved symptom management and quality of life.
Real-time Adjustments
AI’s ability to monitor patient progress and treatment impacts in real-time allows for dynamic adjustments to treatment plans. This approach ensures that patients receive the most effective therapies throughout their treatment journey, addressing any changes in their condition promptly. For example, in managing multiple sclerosis, AI can track disease activity and patient response to medication, enabling clinicians to modify treatment regimens as needed. This real-time feedback loop helps avoid potential side effects and optimizes therapeutic outcomes.
The use of AI for real-time adjustments also extends to postoperative care and rehabilitation for neurological patients. By analyzing data from wearable devices and other monitoring tools, AI can provide insights into patient recovery and suggest modifications to rehabilitation protocols. This continuous, data-driven approach supports a more adaptive and responsive healthcare system, ultimately leading to better patient care. The ability to make real-time adjustments allows for a more proactive stance in managing neurological disorders, catching issues early and making necessary changes before they become more severe.
Future Healthcare Paradigms
Early Diagnosis
AI-enhanced diagnostic tools are paving the way for early diagnosis, which is critical for the successful treatment of neurological disorders. Detecting these conditions at an early stage can lead to more effective management strategies and significantly improved patient prognoses. For diseases like Alzheimer’s and Parkinson’s, early identification enables timely interventions that can slow disease progression and enhance quality of life. AI’s capacity to analyze complex datasets rapidly and accurately means that early markers of disease can be identified with greater precision.
The integration of AI in routine clinical practice also fosters a proactive health monitoring approach. Regular screening facilitated by AI tools can identify individuals at risk, offering opportunities for early intervention and prevention strategies. This paradigm shift from reactive to proactive healthcare places a greater emphasis on maintaining long-term health and mitigating disease impact through early action. As AI continues to develop, its role in early diagnosis will only become more prominent, offering new hope for patients and transforming standard medical practices.
Patient-Focused Healthcare
The advancement of AI in healthcare signifies a move towards a more technologically integrated and patient-focused system. Dr. Vinit Banga underscores AI’s potential to transform how medical professionals approach care, providing timely and precise interventions that were previously unattainable. AI aids in developing a more comprehensive understanding of each patient’s unique medical needs, enabling healthcare providers to deliver personalized and effective treatment plans. This improvement in care not only enhances patient outcomes but also contributes to greater patient satisfaction.
Furthermore, AI facilitates a more continuous and interactive relationship between patients and healthcare providers. Through remote monitoring and telemedicine applications, AI can help track patient health outside traditional clinical settings, ensuring that issues are addressed promptly. This patient-centered approach fosters a more holistic and responsive healthcare system, where the individual needs and circumstances of each patient are prioritized. As AI technologies become more integrated into routine care, they will continue to drive innovations that place the patient at the forefront of healthcare delivery.
Addressing Challenges
Ethical and Practical Hurdles
Despite AI’s promising advancements, challenges such as ensuring data quality, addressing ethical concerns, and integrating AI into clinical practice remain. These issues must be tackled to fully realize AI’s potential in neurological diagnosis and treatment. Data quality is paramount, as inaccurate or incomplete data can lead to incorrect diagnoses or treatment recommendations. Ensuring that AI systems are trained on high-quality, diverse datasets is crucial for their effective application in medical contexts.
Ethical considerations also play a significant role in the deployment of AI in healthcare. Patient privacy, informed consent, and the transparency of AI decision-making processes are critical areas that need careful navigation. The integration of AI must be done in a manner that respects patient rights and builds trust in these new technologies. Additionally, healthcare providers must be adequately trained to use AI tools effectively, ensuring that they complement rather than replace human expertise. Addressing these challenges head-on will be vital for the successful incorporation of AI into everyday clinical practice.
Moving Forward
Artificial intelligence (AI) is rapidly transforming the landscape of neurology, bringing a wave of advancements to how we diagnose and treat neurological disorders. By utilizing cutting-edge technologies, AI significantly enhances the accuracy of diagnoses, accelerates the diagnostic process, and lowers related costs. This evolution is vital in managing chronic conditions such as Alzheimer’s, Parkinson’s, and multiple sclerosis, which impact millions of individuals globally. AI’s integration into healthcare systems offers a promising avenue for substantial improvements in patient outcomes. As machine learning algorithms and AI-driven platforms continue to evolve, they provide health professionals with tools to analyze immense datasets quickly and precisely, identifying patterns that might be missed by human observation. This streamlined approach facilitates early detection and personalized treatment plans, paving the way for more efficient and effective medical care. The burgeoning role of AI in neurology presents an exciting frontier for medicine, promising a brighter future for patients and healthcare providers alike.