The American healthcare system is currently navigating a period of unprecedented transformation, a convergence of high-stakes policy battles, a radical restructuring of the pharmaceutical marketplace, and an urgent, consumer-driven demand for simplicity. Industry leaders are signaling a fundamental pivot away from the convoluted and often opaque practices of the past. At this critical juncture, the core tenets of healthcare delivery, from insurance coverage and drug pricing to the everyday patient experience, are being fundamentally challenged and reshaped. The outcome of these concurrent shifts will determine the accessibility, affordability, and effectiveness of care for millions. The prevailing consensus is that the era of incremental adjustments is over, replaced by a dynamic environment where foundational pillars are either reinforced or dismantled, creating a landscape fraught with both significant risk and profound opportunity for innovation and improvement in how Americans manage their health.
Navigating a Shifting Policy and Pharmaceutical Terrain
The Affordable Care Act at a Crossroads
The stability of the Affordable Care Act (ACA) is under considerable strain, facing a multi-pronged assault that threatens to reverse years of gains in insurance coverage. A primary vulnerability lies in the potential dissolution of enhanced advanced premium tax credits, a development that would almost certainly price healthier individuals out of the market, thereby concentrating risk and triggering a sharp escalation in premiums for those who remain. This financial pressure is compounded by persistent legal and political challenges aimed at the U.S. Preventive Services Task Force (USPSTF). Any erosion of its authority would dismantle mandates for no-cost preventive screenings, a cornerstone of the ACA’s public health strategy. Such a change would inevitably lead to delayed diagnoses of serious conditions, shifting the burden to more complex and costly treatments down the line. Furthermore, the rollback of Medicaid expansion in some states and the proliferation of short-term, limited-duration insurance plans continue to weaken the overall risk pool, siphoning off healthy participants and undermining the economic foundation of the ACA marketplaces.
A Reckoning in Drug Pricing and Transparency
The long-standing, rebate-driven model that has defined pharmaceutical pricing is facing an imminent and decisive reckoning. Industry experts anticipate a seismic shift away from the current system of privately negotiated net prices, which has long obscured the true cost of medications. This movement is expected to result in a material reduction in the list prices of many brand-name drugs, directly impacting the complex web of rebates paid to Pharmacy Benefit Managers (PBMs) and payers. In its place, a more fragmented but transparent market is emerging, presenting patients and providers with a diverse array of new pricing pathways, including direct-to-patient cash options and formally established Maximum Fair Prices. This push for transparency is further accelerated by the maturation of the biosimilars market. Biosimilars are rapidly becoming the new benchmark for evaluating whether PBMs are genuinely aligned with the cost-saving interests of plan sponsors or are merely perpetuating revenue-retention strategies through opaque, rebate-like administrative fees, a critical distinction for employers and unions grappling with the immense challenge of providing affordable health benefits.
Redefining the Patient and Consumer Journey
The Push for a Simplified Healthcare Experience
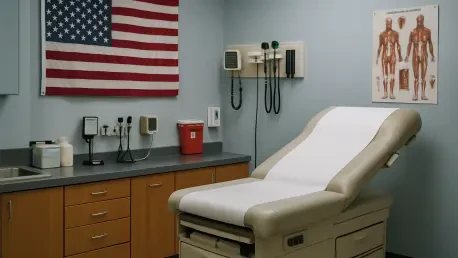
In direct response to overwhelming demand from employers and consumers alike, a powerful movement is underway to make the healthcare system simpler, more affordable, and profoundly more intuitive. As articulated by leaders like Eva Borden of Cigna Healthcare, the central objective is to deconstruct the complexity that has long alienated patients and created barriers to effective care. This initiative involves a fundamental redesign of benefits to reflect real-life situations and priorities, moving away from jargon-laden, one-size-fits-all plans toward models that are easier to understand and navigate. The goal is to empower individuals to make confident, cost-effective decisions about their health without needing to be experts in insurance policy or medical billing. This is being achieved through a combination of clearer communication, streamlined processes, and the strategic use of technology to provide personalized support. The overarching aim is to create a more connected and predictable experience that meets people where they are, whether they are managing a chronic condition, facing a significant medical event, or simply engaging in routine wellness activities.
A New Era of Empowered Health Management
The transformative period in U.S. healthcare culminated in a system fundamentally reoriented around the principles of transparency and user-centric design. The once-impenetrable fortress of pharmaceutical pricing was significantly dismantled, giving rise to a more accountable market where the influence of hidden rebates waned. While the Affordable Care Act weathered significant political and legal storms, the challenges forced a broader conversation about risk pools and the true cost of care, leading to more innovative and localized coverage solutions. Most profoundly, the industry’s pivot toward simplification, driven by technological advancements in data analytics and artificial intelligence, successfully reshaped the patient journey. What emerged was a healthcare experience that was no longer defined by confusion and frustration but by a sense of empowerment, where digital tools and personalized support became standard, enabling individuals to navigate their health decisions with unprecedented clarity and confidence.