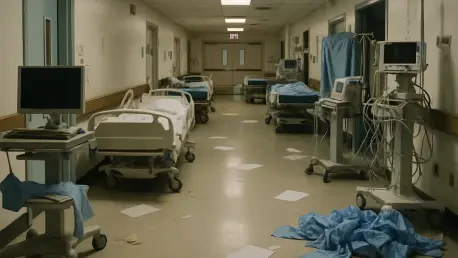
Emergency rooms that once juggled unpredictable nights now confront a predictable shortage that turns routine care into triage, and patients feel the difference in delayed meds, missed checks, and preventable infections. Across Maryland, clinical units are operating too thin to sustain vigilance, and the consequences are measurable in avoidable harm and longer recoveries. When beds remain occupied because treatment stalls or complications emerge, capacity tightens elsewhere, making it harder to admit, transfer, or discharge on time. Health systems are trying to slow the slide with hiring sprees, retention bonuses, and digital monitoring, yet the pattern holds: understaffing invites error, overload breeds burnout, and turnover drains expertise. Breaking the cycle will require rebalancing workloads, strengthening ratios, and rebuilding the pipeline so staffing tracks patient acuity rather than budgetary convenience.
How understaffing harms patients
When clinicians stretch across too many patients, precision yields to speed, and medical decisions suffer from frayed handoffs and incomplete documentation that conceal early mistakes. In these conditions, medication orders are rushed, abbreviations blur, and a missed decimal becomes a dangerous dose that might not be caught for days. Maryland’s incident reports have described wrong-route administrations and procedures that were never intended for a given patient, both more likely in units where alarms compete with call lights and charts go unread. Moreover, inexperienced staff are often floated into unfamiliar specialties, raising the odds of misinterpretation during high-stress moments. Each near miss consumes attention that should go to proactive care, which in turn reduces the bandwidth to double-check orders, reconcile meds, and verify identity before interventions.
Thin staffing also undermines observation, the quiet backbone of safe care that depends on time and focus to notice subtle changes before they escalate. When nurse-to-patient ratios rise, hourly rounding slips from the clock, and a soft wheeze or a new confusion goes unflagged until it becomes respiratory distress or delirium. Diagnostic tests are queued, lab results linger in the inbox, and consults arrive after the window for early intervention has closed. The delays cascade: pain lingers, mobility stalls, and infections take hold, each adding hours and then days to the length of stay. Longer hospitalizations reduce throughput, clogging admissions in the emergency department and creating a feedback loop that intensifies pressure on every subsequent shift. The system becomes slower, not because staff are careless, but because too few hands can only move so fast.
Infection control and neglect risks
Infection control relies on meticulous repetition—hand hygiene at the right moments, cleaning high-touch surfaces on schedule, and isolating patients promptly when risk is suspected—not just on policy binders. With fewer staff on the floor, those routines break down unevenly, and gaps in compliance persist long enough for hospital-associated infections to rise. Surveillance rounds are truncated, peer checks fade, and feedback cycles stretch from hours to days. A missed gown in a hurry or a skipped terminal clean after a transfer becomes the weak link pathogens exploit. Infection preventionists can update protocols and post reminders, but without enough people to do the work consistently, even the best guidance struggles to reach the bedside in real time.
Patients also encounter quieter harms that rarely make headlines yet shape perceptions of safety as surely as lab results. Call lights linger unanswered, water pitchers sit empty, and repositioning schedules slip, increasing the risk of pressure injuries and deconditioning. Families watch these omissions accumulate and infer indifference, even as staff sprint between rooms, trying to juggle tasks that would overwhelm a larger team. Escalations for deteriorating patients are slower when the nurse covering six or seven patients is already managing two fresh admissions and a discharge with complex instructions. These are not lapses of caring; they are the predictable outcome of too many competing priorities. Still, the effect on trust is real, and complaints often translate into legal and reputational exposure.
The vicious cycle behind the crisis
At the center is burnout, an erosion of energy and purpose that comes from giving more than a body and mind can replenish between shifts. Mandatory overtime may keep a unit open tonight, but it extracts tomorrow’s capacity by draining reserves needed for judgment and empathy. High acuity and frequent surges add moral distress when staff know what safe care requires yet lack the hours to deliver it. As seasoned clinicians depart or step into travel roles to regain control over schedules, institutional memory thins. Teams become less cohesive, precepting gets rushed, and small miscommunications multiply, increasing error risk for patients and frustration for colleagues who remain.
Compensation misalignment and training bottlenecks reinforce the spiral. When pay fails to track workload and complexity, clinicians gravitate to employers or regions that offer stability and predictability, creating holes that are hard to fill quickly. Nursing schools and allied health programs face constraints in faculty and clinical placements, slowing graduation even as demand grows. New graduates need structured mentorship to thrive, yet preceptors are stretched and formal development time is the first casualty of a hectic schedule. Add documentation burdens and inconsistent supervision, and the job becomes a maze of clicks and workarounds that obscure the craft of bedside care. Without reliable mental health support and recovery time, resilience programs cannot touch the root causes of exhaustion.
What hospitals are trying now
Health systems are throwing weight behind recruitment: faster onboarding, sign-on packages tied to retention milestones, and more aggressive outreach to clinicians who left during the pandemic’s peak. To stem departures, leaders are easing mandatory overtime, expanding self-scheduling, and creating clear progression paths with differential pay for high-skill roles like critical care, telemetry, and precepting. The intent is straightforward—make staying put competitive with traveling, and make growth at the bedside as respected as moving into management. Some units are piloting team-based models that pair novice and expert nurses to balance workloads and learning, with early signs of better continuity and fewer missed tasks.
Technology and care redesign are also part of the response, though expectations are more measured than in earlier hype cycles. Telehealth consults now bridge gaps in specialty coverage, and virtual nursing stations assist with admissions, education, and discharge coordination, freeing bedside teams for complex care. Real-time analytics flag staffing gaps before they become crises and map patient acuity to allocate resources more precisely. Infection control efforts are being refocused on the fundamentals, with spot audits, on-the-spot coaching, and simplified protocols aimed at consistency over complexity. Even so, the consensus is cautious: digital tools extend reach but do not replace the presence and judgment that only sufficient staffing brings to a bedside at 3 a.m.
Legal and policy pressures
As adverse events climb, malpractice exposure grows, pulling leaders into a delicate balance between transparency, remediation, and risk management. Lawsuits, regulatory investigations, and settlement costs consume attention that otherwise might fund retention packages or expand training cohorts. The pressure can lead organizations to favor short-term optics—new signage, mandatory modules, or task forces—over the structural changes that take months to deliver but actually reduce harm. Yet legal scrutiny has also sharpened focus on measurable levers that tie directly to outcomes, such as enforceable nurse-to-patient ratios that adjust with acuity and documented escalation pathways for high-risk scenarios.
Those levers point toward a practical blueprint that prioritized durable fixes over stopgaps and recognized that safe staffing was not a perk but the foundation of care. Actionable steps included aligning compensation with responsibility and complexity, expanding education capacity through funded faculty lines and paid preceptorships, and protecting time for recovery, mentoring, and continuing education. Maryland’s trajectory mirrored national patterns, but local action still mattered; targeted reforms cut errors, shortened stays, and rebuilt trust when they were applied with persistence rather than in bursts. While technology, wellness programs, and incentives provided essential support, lasting gains came from stabilizing the workforce and matching staffing to the real demands of patients.