Navigating the intricate intersection of health research and privacy rights is no simple task, as it encompasses a spectrum of ethical and legal concerns. Health data security is central to the discourse, with a dual imperative to uphold individuals’ confidentiality while fostering the greater good through medical progress.The ethical quandaries involved are profound. On one hand, the aggregation and analysis of health data can lead to breakthroughs in treatment and understanding of diseases, benefiting society at large. On the other hand, patients entrust their personal health information to researchers with the expectation that their privacy will be fiercely protected.Legislation plays a critical role in this arena, outlining stringent criteria for data handling and stipulating penalties for breaches. Researchers are tasked with designing studies that adhere to these rules while ensuring data integrity and security. Meanwhile, technological advances introduce both opportunities and vulnerabilities – sophisticated encryption techniques can shield sensitive information, but as cyber threats evolve, so must defenses.In striking the right balance, transparency is key. Participants must be well-informed about how their data will be used, the measures in place to safeguard it, and their rights in the research process. Only with a well-structured framework that respects individual privacy and delineates clear ethical guidelines can the harmony between health research gains and privacy be maintained.
Understanding Health Information Privacy
The Essence of Privacy in Health Information
In antiquity, the very crux of healthcare was patient confidentiality, an ideal enshrined in the venerable Hippocratic Oath. Yet, as we’ve ventured into the digital age, the essence of what we consider “privacy” in the medical realm has morphed significantly. Our current milieu, one where electronic sharing is near-instantaneous, renders patient privacy a far more complex affair.Control over the distribution of one’s medical information is now a central focus, given the shifting sands of technology’s impact. On one hand, the digital movement ushers in unparalleled prospects for medical research advancements, offering the promise of insights and breakthroughs powered by the analysis of extensive data pools. On the other, it poses risks that were once unimaginable, challenging our ability to safeguard sensitive personal data effectively.As a result, today’s approach to healthcare privacy must be multifaceted, straddling the line between embracing the potential of technology and respecting the sanctity of individual confidentiality. It is a delicate balancing act, requiring astute attention to privacy’s evolving dynamics and an ongoing conversation about how best to protect the intimate details of one’s health in a world ever more open and connected.
Confidentiality and Security Distinctions
Privacy, while commonly lumped together with confidentiality and security, actually stands distinct from these concepts. Privacy in health data can be seen as the right of individuals to keep their personal health information concealed from others, while confidentiality refers to the responsibility of healthcare professionals to uphold the secrecy of the information entrusted to them. Security, on the other hand, involves the technical and administrative safeguards that protect health data from unauthorized access, breaches, or theft. These three interrelated concepts form a triad that is crucial in the context of protecting health information within research. By distinguishing between them, we can begin to understand the layered approach required to handle sensitive health data responsibly.
Ethical and Social Implications of Privacy
The Intrinsic Value of Privacy
Privacy carries a weight beyond its functional role; it resonates with core human values of dignity, autonomy, and integrity. Respecting an individual’s health information privacy is inherently linked to the ethical principle of nonmaleficence, the avoidance of harm. This respect forms the basis upon which trust between patients and healthcare providers or researchers is built. In a wider context, privacy fosters confidence in health systems and contributes positively to the social fabric by enabling individuals to control personal information, thereby promoting voluntary participation in health research. This fundamental ethical consideration underscores the importance of maintaining privacy in the research domain to ensure the well-being of individuals and, concomitantly, the collective progress of society.
Trust and Public Attitudes Toward Health Data Use
Public attitude toward health data privacy often reflects a dichotomy of trust and skepticism toward medical institutions and research practices. On one hand, there is recognition of the potential for health data to lead to breakthroughs in medicine. On the other, there is an enduring concern over the misuse of personal information, particularly with frequent reports of data breaches in the media. These concerns emphasize the need for transparency and consent mechanisms that respect the individual’s desire to control the use of their health information. Understanding these public sentiments is key for researchers and policymakers alike—to ensure that health research can continue without compromising the trust and willingness of individuals to participate in studies that ultimately aim to benefit us all.
Legal Protections for Health Information Privacy
Historical Overview and HIPAA’s Role
The protection of health information in the United States has seen significant evolution over the past few decades. Initially, privacy was a matter of professional ethics, exemplified by the Hippocratic Oath. As technology evolved and digitization became commonplace, the need for formal legislation became evident. The pivotal legislation in this arena is the Health Insurance Portability and Accountability Act (HIPAA) of 1996. HIPAA’s Privacy Rule was a response to growing concerns around the privacy of health information, creating national standards for its protection. The rule mandates controls on the use and dissemination of protected health information (PHI), although it has faced criticism for not fully addressing the intricacies of digital information flow. Nevertheless, its introduction marked a significant advancement in the establishment of privacy rights concerning health data.
The Variability of Protections Across Jurisdictions
Navigating health information privacy laws in the U.S. is akin to traversing a complex maze due to the disparate legal protections across states. Beyond the federal HIPAA standards, states like California have gone a step further with laws like the Confidentiality of Medical Information Act, providing even stronger safeguards for personal health information. In contrast, some states might offer less substantial protections.This uneven landscape poses significant challenges for various stakeholders. Healthcare professionals, researchers, and patients must acquaint themselves with the intricacies of differing privacy regulations, which can affect everything from consent procedures to data breach notifications and the right to access personal health records. This divergence reflects the struggle in creating unified, adaptive policies in an era where technological change is rapid and expectations of privacy are diverse. Balancing state-specific health privacy laws while maintaining a consistent national standard remains an ongoing puzzle for policymakers, as they strive to protect patient privacy without stifling innovation or healthcare delivery.
Risks and Challenges in Health Data Security
Potential Harms from Data Breaches
The transition to digital health records has significantly enhanced the management and analysis of patient data. However, this shift has also laid bare a host of security concerns. Cybersecurity incidents in the health sector can lead to a wide spectrum of negative outcomes, which include not only direct financial repercussions but also damage to institutional reputations and the mental well-being of the individuals whose data has been compromised. The more severe consequences of security lapses might involve prejudicial treatment or the marginalization of those affected.As health data breaches can have such severe and diverse consequences, the urgency for robust and impervious digital defenses is paramount. Healthcare organizations and professionals must proactively keep pace with the ever-changing landscape of cyber threats. This involves deploying advanced security infrastructure and enacting stringent procedures to safeguard against unauthorized access and data loss, while concurrently supporting bona fide health research initiatives.The balance between data accessibility for research purposes and privacy protection is delicate; hence, continuous vigilance is imperative. Security protocols must be dynamic, evolving in step with both technological advancements and emerging threats. Through these means, the integrity of health data can be preserved, and the trust of patients and the public can be maintained.
Gaps in Protection and Compliance
The current landscape for health information protection is riddled with shortcomings despite the HIPAA Security Rule’s intentions. Regulatory oversight often misses the mark, and the rapid evolution of technology exposes gaps in these frameworks—gaps that could be manipulated to the detriment of patient privacy. To bridge these vulnerabilities, healthcare entities must go beyond basic security protocols. They are tasked with the imperative of continuously refining their defenses through thorough and regular audits, reviews, and system updates.Yet, this burden of bolstering information safety isn’t for healthcare institutions to bear alone. Participation from diverse actors within the health research domain, inclusive of government bodies, academic and private research institutions, as well as the researchers themselves, is crucial. Unified efforts are required to navigate the complexities of health information security in an era where digital innovation outpaces regulatory adaptation.Strategically addressing these inadequacies remains pivotal to uphold the confidence of the general public. The healthcare sector’s commitment to this never-ending improvement cycle is fundamental in ensuring that sensitive health data is sheltered from the myriad of threats it faces in the digital age. Only through such collective and rigorous dedication can we aim to secure the sanctuary of health information.
Technological Innovations and Privacy
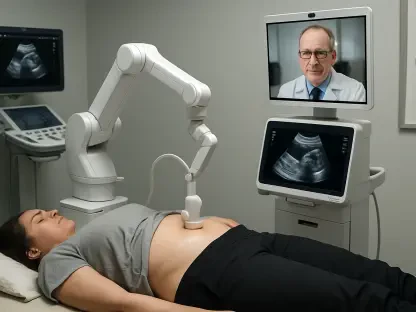
Enhancing Data Privacy with Emerging Technologies
In the realm of health research, safeguarding patient privacy while leveraging data for insights is paramount. Cutting-edge technologies are at the forefront of this balancing act, offering novel methods to protect sensitive health information. Privacy-preserving data mining is one such innovation, enabling researchers to delve into data without compromising personal details. Meanwhile, advancements in personal digital health record systems grant individuals greater control over their medical information. These platforms not only secure their data but also allow for selective sharing for research or clinical purposes.This technological stride towards secure, patient-empowered data management heralds a new era in health research. Individuals can now participate more actively in their health care journey, dictating who can access their data and for what reasons. Consequently, researchers can conduct studies with rich datasets while upholding strict privacy standards.Employing these technologies requires meticulous implementation to ensure they serve their protective functions effectively. Only with robust safeguards in place will the promise of these emerging tools be fully realized, striking an optimal balance between research advancement and the preservation of privacy in the digital health age.
The Limitations and Considerations of Technology in Privacy
While technology offers new frontiers for health data privacy, it is not without its caveats. For instance, the complexity of privacy-preserving technologies may present a barrier to widespread adoption, especially in regions with limited resources. There is also the risk that enhanced security measures could inadvertently hinder the collaborative nature of health research. Furthermore, the rapid pace at which technology evolves necessitates continuous evaluation and adaptation of privacy measures. Careful consideration must be given to the balance between the long-term benefits and the immediate challenges these technological solutions present, with the overarching goal of prioritizing the individual’s right to privacy while advancing public health objectives.In conclusion, ensuring the privacy and security of health data in research is a task that requires an inclusive approach, sensitive to the evolving technological landscape, the variability of legal protections, and the diverse concerns of the public. By understanding and addressing these factors, the research community can build a framework that not only safeguards privacy but also engenders trust and participation, which are essential for the continued progress of medical research.