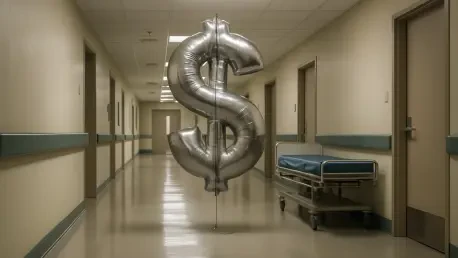
A significant transformation is underway within the financial corridors of American hospitals, as the primary drivers of supply chain inflation are pivoting away from the long-standing concern of pharmaceutical prices toward the rapidly escalating costs of technology and purchased services. A recent forecast from a leading healthcare data firm reveals that over the next 18 months, health systems will grapple with an accelerated rate of overall price increases, largely fueled by sectors far removed from the pharmacy. This shift presents a complex new set of challenges for healthcare administrators, forcing a reevaluation of traditional cost-containment strategies and demanding a more nuanced approach to financial management. As some cost pressures begin to ease due to market competition and policy reforms, others are surging, creating a divergent economic landscape that requires both agility and strategic foresight from hospital leadership to navigate successfully. The data projects an overall market price increase of 2.78% across the entire healthcare supply chain for the period between July 2026 and June 2027, an uptick from the 2.41% inflation rate predicted just six months prior, signaling a new and urgent financial reality.
The New Inflationary Landscape
The latest projections for hospital expenditures paint a picture of uneven and accelerating cost pressures, demanding a closer look at the specific categories driving this new wave of inflation. While the overall increase is noteworthy, the true story lies in the divergence between different segments of the hospital supply chain. The data clearly indicates that the most significant price hikes are occurring in areas outside of direct medical products, forcing a strategic shift in how financial officers approach budget management and cost control. This section will dissect the components of this new inflationary environment, exploring the surge in indirect costs and the contrasting moderation in the pharmaceutical sector.
Surging Indirect Costs and Technology’s Role
The primary engine behind the forecasted acceleration in healthcare supply chain inflation is a substantial 3.85% price hike anticipated for indirect spending and purchased services. This figure stands in stark contrast to the more modest 2.32% estimated increase for medical products, highlighting a critical shift in where financial pressures are mounting for health systems. This surge in indirect spending is not a monolithic trend but is instead fueled by significant price increases across a range of essential, non-clinical categories. The technology sector emerges as the most prominent driver, with a forecast indicating a 5.66% rise for IT hardware and software and a 4.5% increase for IT services. These costs reflect the growing reliance on digital infrastructure, electronic health records, cybersecurity, and data analytics in modern healthcare delivery. The ripple effect of broader economic forces is also evident, as persistent issues such as tariffs impacting raw materials and widespread labor cost increases continue to exert upward pressure on prices for everything hospitals procure.
Beyond the digital domain, other critical areas of indirect spending are also contributing to the inflationary pressure, creating a multifaceted challenge for hospital administrators. The forecast details notable price increases for nonmedical capital equipment, which is expected to rise by 4.15%, impacting everything from office furniture to maintenance machinery. The construction sector, vital for facility upgrades and expansions, is projected to see a 3.7% cost increase, while even fundamental supplies like food are expected to become 3.63% more expensive. This broad-based inflation across purchased services and non-clinical goods means that cost-containment efforts must now extend far beyond the traditional focus on medical and surgical supplies. Hospitals are now compelled to scrutinize contracts and manage utilization for a wide array of services and products that, while not directly related to patient care, are indispensable to the day-to-day operations of a modern healthcare facility and are now a primary source of financial strain.
Moderating Pharmaceutical Price Pressures
In a significant departure from long-standing trends, the report predicts a notable tempering of pharmacy price inflation. The projected price change for pharmaceuticals is now 2.84%, a considerable decrease from the 3.35% increase that was forecasted in the previous reporting period. This slowdown can be attributed to a confluence of powerful market and regulatory forces that are beginning to exert downward pressure on drug costs. One of the primary factors is the implementation of federal drug pricing reforms, most notably the Medicare Drug Price Negotiation Program. This landmark policy is starting to impact the pricing of high-expenditure drugs, such as the widely prescribed anticoagulant apixaban (Eliquis), by allowing Medicare to directly negotiate prices with manufacturers for the first time. The effects of such policies are creating a more competitive and transparent pricing environment, providing some relief to hospital budgets that have long been strained by the relentless rise in pharmaceutical expenditures.
The moderation in drug price inflation is further supported by the growing influence of market competition, particularly from the introduction of new biosimilars. These products, which are highly similar to and have no clinically meaningful differences from existing FDA-approved biologic medicines, are challenging the market dominance of some of the most expensive drugs on the market. The report highlights the impact of biosimilars for high-spend drugs like adalimumab (Humira), used to treat autoimmune conditions, and ustekinumab (Stelara), for psoriasis and Crohn’s disease. As more of these lower-cost alternatives become available, they introduce direct price competition that forces down the cost of the original branded products. However, despite this welcome moderation, it is crucial to recognize that pharmaceuticals remain the single largest and fastest-growing component of a hospital’s non-labor expenses. This reality underscores that while the rate of increase may be slowing, managing pharmacy costs will continue to be a critical priority for health systems.
Navigating the New Financial Realities
The divergent trends in hospital inflation—with technology and service costs accelerating while pharmaceutical price growth slows—necessitate a fundamental rethinking of financial strategy. Health systems can no longer rely on a one-size-fits-all approach to cost management. Instead, they must adopt more sophisticated and targeted strategies that address the unique dynamics of each spending category. This new reality demands a proactive and data-driven approach, moving beyond simple price negotiations to a more holistic understanding of value and total cost of ownership across the organization’s entire supply chain.
Beyond Traditional Cost Containment
In this complex and non-uniform inflation environment, traditional cost-containment strategies, which have historically focused on negotiating lower unit prices with suppliers, are proving to be insufficient. The divergence in cost pressures requires a more sophisticated and multifaceted approach to protect financial margins. To effectively manage rising expenses, particularly in the tech and services sectors, hospitals must now integrate their contracting efforts with robust utilization management programs. This involves not just securing a good price on a product or service but also ensuring it is used appropriately and efficiently throughout the organization. Furthermore, a renewed emphasis on product standardization is essential. By reducing the number of different products used for the same clinical purpose, hospitals can increase their purchasing power, simplify inventory management, and reduce waste. This strategy is particularly relevant for medical supplies but can also be applied to technology hardware and software licenses to streamline operations and lower long-term costs.
The most critical evolution in strategy, however, is the adoption of a total cost-of-ownership (TCO) analysis for major purchases. This approach moves beyond the initial acquisition price to consider all associated costs over the lifetime of an asset or service contract. For IT systems, a TCO analysis would include not only the upfront hardware and software costs but also expenses related to implementation, training, maintenance, upgrades, and eventual decommissioning. By evaluating the full financial impact, health systems can make more informed purchasing decisions that deliver better long-term value, even if the initial price is not the lowest available. This holistic view is paramount for managing the escalating costs of technology and other purchased services, enabling leaders to identify hidden expenses and allocate resources more effectively. As one expert from the reporting firm articulated, the key challenge for hospital leaders is to manage this divergence, reallocating focus and resources as some costs accelerate while others moderate, demanding a more strategic and analytical approach to procurement.
The Strategic Imperative for a New Era
The shifting landscape of hospital expenses ultimately demanded a new level of strategic acumen from healthcare leaders. The core challenge they faced was not simply cutting costs, but adeptly managing a complex portfolio of expenses where pressures were simultaneously rising in some areas and easing in others. This environment required a deliberate reallocation of resources and analytical focus. Financial and supply chain executives found that the expertise they had honed over decades in negotiating pharmaceutical contracts had to be redirected and adapted to tackle the intricate and rapidly evolving costs associated with IT infrastructure, service agreements, and capital equipment. The situation underscored that a passive approach to budgeting was no longer viable. Instead, organizations that thrived were those that implemented dynamic financial models and fostered a culture of continuous analysis, allowing them to anticipate cost trends and adjust their strategies proactively rather than reactively. The era had cemented the need for a more integrated approach, where clinical, operational, and financial leaders collaborated to assess the total value and cost of every major investment, ensuring that spending decisions aligned with the institution’s long-term strategic and clinical goals.