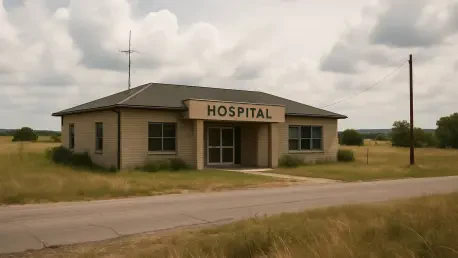
In the current healthcare landscape, the implementation of H.R.1, also known as the Big Beautiful Bill, presents significant questions about the future of rural hospitals and healthcare access across the United States. The Republican-controlled Congress has passed this sweeping legislation, which many argue threatens to destabilize critical healthcare systems, particularly in rural areas. At a time when access to quality healthcare is paramount, the potential ramifications of this new law warrant close examination. Key issues under scrutiny include reduced Medicaid funding, increased operational costs for hospitals, and diminished protections that previously ensured coverage for vulnerable groups. As hospitals struggle under financial constraints, communities worry about their access to essential health services. This legislation thus signals a turning point for hospitals and clinics that serve as lifelines in under-resourced areas, raising crucial questions about the broader implications for public health and healthcare equity in the nation.
Legislative Consequences on Healthcare Access
H.R.1’s passage has cast a spotlight on the precarious state of healthcare access, especially in rural areas where hospitals like Petaluma Valley Hospital (PVH) play pivotal roles. This law has ushered in contentious changes, notably cutting Medicaid spending—an essential source of financial support for these institutions. The impact is projected to be vast, potentially leading to a staggering 11.8 million people losing their health coverage. This includes lower-income adults, children, veterans, and those with disabilities who rely on Medicaid and other support systems. As healthcare access becomes more restricted, the specter of uncompensated care looms large over hospitals, burdening providers with the task of caring for uninsured patients without corresponding financial reimbursement. Elece Hempel, a dedicated advocate for community health services, has emphasized the imminent challenges rural hospitals face, illustrating the dire need for systemic reform.
These legislative decisions underline a broader concern about the uneven effects of policy changes, as rural healthcare systems contend with rising demands and diminishing resources. The landscape is one where providers and patients alike must navigate uncertainties ushered in by this legislation. Moreover, the scaling back of nutritional support services compounds these issues, further stressing communities that depend on integrated health services for overall well-being. As rural hospitals brace for the upcoming challenges, the intersection of legislative decisions and healthcare access remains a critical focal point in the ongoing debate over the future of the American healthcare system. This scrutiny brings into sharp focus the vulnerabilities within these communities and raises alarms about potential health emergencies resulting from inadequate access to care.
Financial Strain on Rural Hospitals
Beyond access, H.R.1 introduces significant financial challenges that threaten the sustainability of rural hospitals. Institutions such as PVH are emblematic of the overwhelming difficulties posed by slashed Medicaid reimbursements, which make up a substantial portion of their operational revenue. Hospitals in these settings are often financially fragile, relying heavily on government funding to remain viable. The law not only strains their finances but also exacerbates existing operational challenges, including increasing labor costs and resource management inefficiencies. Providence Health, PVH’s parent organization, reflects this nationwide crisis with alarming operating losses in recent fiscal years. This scenario is mirrored by countless hospital networks nationwide, indicating a systemic issue that questions the viability of rural healthcare facilities.
Moreover, the repercussions of these financial constraints call for urgent federal healthcare reform. Institutions are forced to grapple with the complexities of maintaining service quality while navigating reduced funding and expanding needs. Austerity measures may result in workforce reductions, further complicating the delivery of care. This is particularly pressing as anti-immigrant policies disrupt the staffing of crucial roles, including nursing and caregiver positions. The strain on resources and staffing poses significant threats to care standards, leaving hospitals in a vulnerable position, unable to effectively serve their communities’ health needs. Addressing these challenges requires comprehensive policy interventions and constructive dialogue between stakeholders to ensure supportive measures for maintaining hospital operations and safeguarding community health.
The Broader Socio-Political Impact on Healthcare
H.R.1’s implications extend beyond financial and operational burdens, touching upon deeper socio-political issues within the healthcare system. Critics argue that the prioritization of tax cuts for affluent individuals has come at the expense of the healthcare and social safety nets essential for millions of Americans. This political landscape creates friction as resources are reallocated, often resulting in constraints that disproportionately affect the most vulnerable populations. These insights are keenly reported by industry commentary and highlight the disjunction between policy decisions and their practical impact on the ground. The legislation’s focus showcases a broader trend of how political decisions intersect with public health priorities, signaling a shift that could drive systemic changes in healthcare accessibility.
In response, hospitals and communities are prompted to seek innovative solutions to the legislative challenges at hand. Many hospitals are striving to adapt by investing in infrastructure enhancement and community health initiatives, aspiring to build resilience against current and future challenges. For instance, hospitals have made significant improvements by modernizing facilities and equipment, which positions them better in addressing community health needs. Programs like the “Blue Zones” initiative also underscore efforts to enhance lifestyle-related outcomes, fostering a community-oriented approach to health. Despite these strides, the shadow of legislative hurdles persists, urging communities to advocate for equitable healthcare delivery actively. This advocacy forms the linchpin in discussions about the future sustenance and transformation of rural healthcare services.
Calls for Reform and Community Engagement
As challenges mount, calls for comprehensive reforms and concerted community engagement become increasingly pivotal. The advocacy for rural hospitals, particularly those like Petaluma Valley Hospital, emphasizes the necessity for a robust healthcare framework that includes systemic reforms and sustained funding. Supporters of such initiatives argue for the importance of grassroots activism and legislative advocacy to counteract the adverse effects of H.R.1. By galvanizing community backing, these efforts intend to maintain essential healthcare services pivotal to the well-being of rural populations. Paramount in these discussions is the need to address chronic underinvestment in rural health infrastructure and explore innovative funding and service delivery models.
These reformative efforts harness collective community spirit, with stakeholders recognizing the importance of retaining hospitals as vital community assets. Local engagement and advocacy propel initiatives that seek strategic alliances with policymakers, striving to secure necessary funding and policy changes. Furthermore, these grassroots movements emphasize the need for broader public discourse around healthcare priorities and the socio-economic implications of legislative decisions. The current climate underscores a critical moment for stakeholders at all levels to reassess and recalibrate policies towards a more sustainable model that prioritizes comprehensive healthcare access. The momentum gained could serve as a catalyst for wider-reaching reforms that ensure equitable and quality healthcare irrespective of geographical and socio-economic barriers.
Conclusion and Future Considerations
In the evolving healthcare landscape, the enactment of H.R.1, otherwise referred to as the Big Beautiful Bill, raises significant concerns about the future of rural hospitals and healthcare access in the United States. Passed by a Republican-majority Congress, this extensive legislation is said by many to pose significant risks to the stability of vital healthcare systems, especially in rural regions. Now, when access to quality healthcare is more crucial than ever, this new law’s potential effects deserve careful analysis. Key areas of concern include curtailed Medicaid funding, rising operational costs for hospitals, and lessened safeguards that once ensured coverage for vulnerable populations. As hospitals grapple with financial hardships, communities face anxiety over their ability to obtain necessary health services. This legislation thus marks a crucial moment for hospitals and clinics, which serve as vital resources in underserved areas. It prompts essential discussions about the wider effects on public health and healthcare equity across the nation.