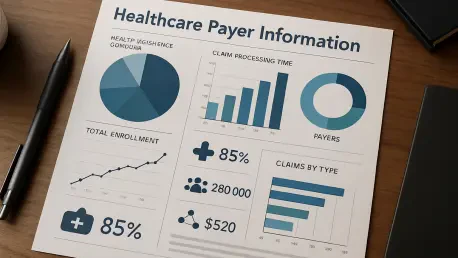
The healthcare payer information technology sector is rapidly approaching a defining moment, with 2026 poised to be a pivotal execution year that will fundamentally reshape investment priorities, technological roadmaps, and the entire vendor acquisition landscape. A powerful convergence of stringent federal compliance deadlines and a strategic industry-wide shift toward outcomes-driven healthcare is forcing a profound modernization of payer technology stacks. Payer organizations, from commercial insurers to Medicaid and Medicare Advantage plans, are moving beyond the siloed task of meeting regulatory requirements. Instead, they are prioritizing investments in advanced IT platforms capable of simultaneously achieving compliance, reducing administrative friction, enhancing cybersecurity, and, most critically, delivering measurable improvements in both patient care and the total cost of care. This dual mandate is sparking a new acquisition race for platforms that can demonstrably shorten time-to-treatment, close gaps in care, and improve quality performance, transforming compliance from a cost center into a catalyst for value creation.
The Regulatory Gauntlet Driving Technological Transformation
The most significant catalyst for this market-wide transformation is the CMS Interoperability and Prior Authorization Final Rule, which is moving from policy theory to operational reality. For 2026, payers are intensely focused on achieving readiness for the rule’s demanding prior authorization requirements, which include implementing stricter decision timeliness, ensuring enhanced transparency in all communications, and preparing for new public reporting mandates. This work must be executed with precision to avoid inadvertently creating new barriers to patient access. In parallel, 2026 represents a critical build-and-harden year for the required Fast Healthcare Interoperability Resources (FHIR)-based API infrastructure. This foundational technology must be robustly in place to support the rule’s expanded payer data exchange capabilities, which become mandatory in 2027. This regulation directly connects complex IT modernization efforts to tangible patient impact by mandating a reduction in care delays and administrative burdens for clinicians, creating substantial opportunities for vendors offering interoperability platforms, PA workflow automation, and sophisticated API management solutions.
While the prior authorization rule commands significant attention, a constellation of other regulatory developments is adding to the pressure for comprehensive modernization. The ongoing Transparency in Coverage requirements continue to mature, demanding greater operational sophistication from payers. The technology focus in 2026 is on scaling and fortifying the data pipelines responsible for publishing, validating, and hosting complex machine-readable files, with an eye toward anticipated agency direction on new prescription drug reporting complexities. Simultaneously, the Advanced Explanation of Benefits mandate under the No Surprises Act remains a key strategic priority. Although near-term enforcement dates are not set, payers are proactively investing in foundational capabilities like real-time benefits verification and accurate cost-estimation tools. Furthermore, continuous policy and technical changes for Medicare Advantage and Part D plans for the 2026 contract year reinforce the need for constant operational refinement of systems supporting regulatory reporting, quality measurement analytics, and member communications. Capping this off are proposed updates to the HIPAA Security Rule, which signal a heightened cybersecurity standard and are accelerating investment in security risk analysis, end-to-end encryption, and advanced incident response tooling.
The New Acquisition Race for Value-Driven Platforms
These intense regulatory pressures are fueling several overarching technology trends and creating a dynamic mergers and acquisitions environment where value is defined by impact. Payers are orchestrating a widespread shift away from manual, fax-based prior authorization processes toward automated, API-driven workflows that leverage standardized data exchange and provide measurable performance metrics on approval turnaround times. This evolution is underpinned by the rise of interoperability-by-default architectures, where the expansion of FHIR-based API programs is becoming foundational. These programs require sophisticated identity matching, granular member consent controls, and robust data governance to support secure and compliant data exchange at scale. At the same time, cybersecurity has been elevated from a back-office function to a strategic, board-level priority focused on enterprise-wide controls alignment, auditability, and proactive security engineering built into the development lifecycle. The use of governed AI and machine learning is also expanding in areas like fraud detection and payment integrity, but it is now paired with strong frameworks that demand model risk management, explainability, and robust privacy controls to ensure ethical and effective deployment.
This new reality is sparking a fierce acquisition race for IT platforms that directly address the dual challenges of compliance and outcomes, with strategic investment intensifying around assets that convert regulatory obligations into measurable clinical and financial value. The most attractive acquisition targets will be companies whose platforms demonstrate scalable interoperability, auditable automation, and quantifiable improvements in care quality and affordability. Key categories include prior authorization modernization platforms that demonstrably reduce approval cycle times and administrative burdens for providers. Also in high demand are vendors providing FHIR-native interoperability enablement tools, such as API gateways, identity resolution services, and consent management solutions. Buyers will also prioritize impact-driven care management platforms that use data to stratify populations and trigger closed-loop interventions with documented outcomes. This M&A focus extends to integrated medication access technologies that streamline complex workflows for specialty drugs and actionable home-based care platforms that ensure remote monitoring alerts trigger tangible clinical interventions.
Charting a New Course for Healthcare Value
The healthcare payer IT market in 2026 was ultimately defined by execution and accountability. The convergence of pressing regulatory deadlines and an industry-wide imperative to improve health outcomes forced a profound and necessary modernization of payer technology stacks. The most successful payers and vendors were those who successfully aligned their strategies and solutions to this new reality. They deployed platforms that were not only compliant by design but were also capable of delivering the measurable improvements in access, quality, and affordability that the modern healthcare ecosystem demanded. This strategic alignment did more than satisfy federal mandates; it laid the groundwork for a more responsive, efficient, and patient-centric healthcare system.