In a world where cancer remains one of the most formidable health challenges, a groundbreaking innovation in particle therapy is offering new hope for patients and clinicians alike. Emerging from the labs of Germany’s GSI/FAIR accelerator facility in Darmstadt, researchers with the BARB (Biomedical Applications of Radioactive Ion Beams) project have developed a transformative approach using carbon-11 (11C) ion beams. This technology not only delivers precise radiation doses to tumors but also enables real-time visualization of the beam’s path through positron emission tomography (PET). By addressing the critical issue of range uncertainty in cancer treatment, this dual-purpose method promises to enhance the accuracy of targeting tumors while significantly reducing the risk of damage to surrounding healthy tissues. The implications of this advancement are profound, potentially reshaping how radiation therapy is administered and monitored, and offering a safer, more effective path for millions battling cancer across the globe.
Overcoming Precision Barriers in Particle Therapy
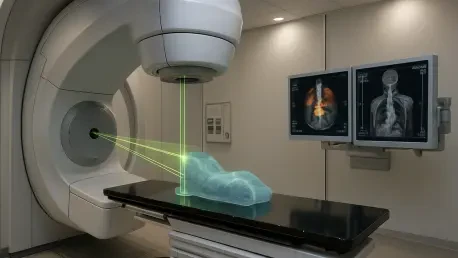
Particle therapy stands out as a highly precise cancer treatment, utilizing protons or heavy ions to focus radiation doses on tumors through a phenomenon known as the Bragg peak, where energy release peaks at a specific depth. Despite this advantage, the method has long grappled with range uncertainty, where even slight miscalculations in beam placement can shift the Bragg peak, either missing the tumor or harming adjacent healthy structures. Traditional carbon-12 (12C) beams, commonly used in this therapy, provide limited feedback during treatment, as the PET signals from their fragments are weak and often misaligned with the intended dose area. This gap in real-time data has hindered clinicians’ ability to ensure pinpoint accuracy, often necessitating wider safety margins that can compromise effectiveness or safety. The persistent challenge of aligning the therapeutic dose precisely with the tumor’s location has driven the search for innovative solutions that can bridge this critical gap in particle therapy applications.
The introduction of radioactive ion beams, particularly 11C, marks a significant leap forward in addressing these precision challenges. Unlike their non-radioactive counterparts, 11C beams serve a dual role: they deliver a targeted therapeutic dose while emitting positrons that can be detected via PET imaging, providing a clear, real-time view of the beam’s position within the body. This stronger and more accurate PET signal minimizes the discrepancy between the dose and activity peaks, allowing for immediate adjustments during treatment if needed. Such capability reduces the reliance on pre-treatment assumptions and enhances confidence that the radiation is striking the intended target. By narrowing safety margins around tumors, this approach not only boosts the likelihood of successful outcomes but also protects vital organs and tissues from unintended exposure, setting a new standard for precision in radiation-based cancer care.
Groundbreaking Results from Experimental Trials
Experimental trials conducted under the BARB project have yielded promising results that underscore the potential of 11C ion beams in cancer treatment. Focusing on mice with osteosarcoma tumors positioned near the spine, researchers employed a specialized small-animal PET scanner to monitor the beam’s trajectory during therapy sessions at the GSI/FAIR facility. The outcomes were remarkable, with higher doses achieving complete tumor control and lower doses resulting in substantial growth delays, all while preserving the integrity of the nearby spinal cord. This level of precision demonstrates the technology’s capacity to target malignant growths effectively without inflicting collateral damage on critical anatomical structures. Such findings are a testament to the power of integrating treatment with imaging, offering a glimpse into how this method could transform clinical practices for human patients facing similar tumor locations and treatment challenges.
Beyond the immediate success in tumor targeting, these experiments revealed unexpected biological insights that could redefine understanding of high-dose radiotherapy effects. A notable observation was the dose-dependent washout of the radioactive 11C signal from the treated tumors. At lower doses, the signal diminished rapidly, likely due to blood flow clearing the isotopes from the area, but at higher doses, this rapid washout ceased entirely. This pattern suggests that elevated radiation levels may impair the blood vessels feeding the tumor, effectively cutting off its nutrient supply as a therapeutic mechanism rather than solely destroying cancer cells directly. This discovery opens up new avenues for research into how vascular damage contributes to treatment efficacy, potentially influencing future strategies in particle therapy to maximize impact on tumors while minimizing harm to surrounding healthy environments, thus refining the overall approach to radiation delivery.
Future Horizons for Radioactive Beam Technology
As the BARB project continues to push boundaries, attention is shifting toward exploring additional radioactive isotopes like carbon-10 (10C) and oxygen-15 (15O), which could offer even stronger PET signals and improved temporal resolution for imaging during treatment. The development of the Super-FRS fragment separator at FAIR is poised to facilitate these studies by providing the high-intensity beams required for rigorous testing. Such advancements aim to fine-tune the balance between therapeutic effectiveness and imaging clarity, ensuring that the technology can adapt to a variety of tumor types and locations within the body. By expanding the range of isotopes under investigation, researchers hope to uncover optimal combinations that enhance both the precision of dose delivery and the quality of real-time feedback, ultimately broadening the applicability of radioactive ion beams in diverse medical scenarios.
Translating this cutting-edge technology into clinical settings remains a key focus, with significant efforts directed at overcoming logistical and financial barriers. Collaborative initiatives, such as CERN’s MEDICIS-Promed project, are developing cost-effective production methods for radioactive isotopes using isotope separation online (ISOL) techniques, while GSI is innovating accelerator designs tailored for medical applications. These endeavors reflect a collective determination to make radioactive ion beam therapy accessible to hospitals worldwide, ensuring that the benefits of enhanced precision and safety are not confined to research labs. By addressing the practical challenges of scalability and affordability, the medical physics community is laying the groundwork for a future where this revolutionary approach becomes a standard tool in the fight against cancer, offering renewed hope to patients through safer and more targeted treatment options.
Reflecting on a Path Forward for Cancer Care
Looking back, the strides made by the BARB project with 11C ion beams represent a pivotal moment in the evolution of particle therapy. The ability to simultaneously treat and image tumors with unprecedented accuracy tackled a fundamental flaw in radiation delivery, as evidenced by successful tumor control in animal models without compromising nearby critical structures like the spine. Fascinating biological revelations, such as the potential role of vascular damage in high-dose effects, added depth to the understanding of radiotherapy mechanisms. As the journey unfolds, the push to test new isotopes and develop cost-effective technologies underscores a commitment to clinical integration. Moving forward, the focus should center on accelerating partnerships between research institutions and healthcare providers to streamline adoption, while investing in training for medical professionals to handle these advanced tools. Such steps will ensure that the promise of radioactive ion beams translates into tangible benefits for cancer patients globally.