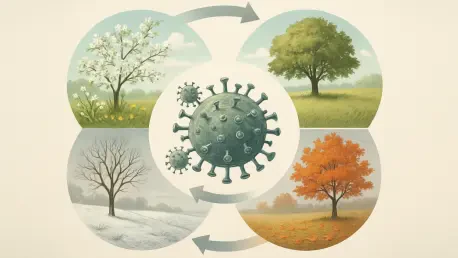
Infectious diseases often follow a surprisingly predictable calendar, with outbreaks of illnesses like influenza and dengue fever recurring at the same time each year like clockwork. This phenomenon is driven by seasonal epidemiology cycles, which are the rhythmic fluctuations in disease transmission shaped by a complex interplay of environmental, behavioral, and biological factors that create ideal windows for pathogens to thrive. By deconstructing why certain viruses surge in the winter or why mosquito-borne illnesses peak during rainy seasons, public health experts can shift from a reactive to a proactive stance. This understanding allows for the development of sophisticated, science-driven strategies that anticipate and mitigate the next outbreak before it takes hold, transforming public health from a practice of response to one of prediction and prevention, ultimately saving resources and protecting communities more effectively.
The Core Drivers of Seasonality
The engine behind these predictable cycles is the precise alignment of environmental conditions that favor pathogen survival and human vulnerability. For many respiratory illnesses, the cold, dry air of winter serves as a primary catalyst. Lower temperatures and absolute humidity enhance the viability of viruses like influenza, allowing viral particles to remain stable for longer periods in the air and on surfaces. This dry air also compromises the human body’s first line of defense by weakening the mucosal barriers in the nasal passages, making viral entry easier. In stark contrast, warmer and wetter conditions foster the spread of vector-borne diseases. Seasons characterized by increased rainfall lead to the proliferation of standing water, which provides ideal breeding grounds for vectors like the Aedes and Anopheles mosquitoes, the carriers of dengue and malaria, respectively. This direct link between climate and vector populations synchronizes disease outbreaks with specific seasons, particularly in tropical and subtropical regions.
Human behavior acts as a powerful amplifier for these environmental factors, often creating the perfect storm for transmission. During colder months, people naturally spend more time indoors, leading to increased crowding in homes, schools, offices, and public transportation. This heightened level of close contact dramatically accelerates the spread of respiratory pathogens, contributing to the explosive peaks seen in winter. The school calendar is a particularly potent driver, concentrating children, who are often highly efficient transmitters of infectious diseases, in enclosed spaces during the fall and winter. Furthermore, human mobility patterns, such as increased travel during holidays, coincide with peak transmission seasons and act to seed outbreaks across different communities and even continents. This dynamic helps synchronize epidemics on a much larger scale, turning what might have been localized flare-ups into widespread public health events that demand a coordinated response.
The Predictable Dynamics of an Outbreak
A hallmark of seasonal diseases is their remarkable ability to persist at low, often endemic levels during their off-season, sometimes within animal reservoirs or asymptomatic human carriers. When the right environmental, behavioral, and biological conditions finally align, this low-level transmission rapidly amplifies, leading to a synchronized epidemic peak. This resonance in epidemiology cycles explains phenomena like the predictable global influenza waves that sweep through the Northern and Southern Hemispheres at opposite times of the year, following the seasons as they shift across the globe. The timing and nature of these cycles are also heavily influenced by geography. Temperate zones typically experience sharp, concentrated surges in respiratory infections during the winter months. In contrast, equatorial regions may see bimodal cycles for diseases like cholera, with peaks corresponding to their two distinct rainy seasons, underscoring how these cycles adapt to local ecological and climatic conditions.
The severity of a seasonal outbreak can also be influenced by these recurring factors, determining whether a season will be mild or severe. For instance, population immunity is often at its lowest during peak seasons due to factors like winter vitamin D deficiency and the physiological stress associated with colder weather, which can lower resistance and prolong epidemics. In the case of vector-borne diseases, the intensity of rainfall can trigger exponential growth in mosquito populations, overwhelming control efforts and leading to more severe and extended outbreaks. These principles are clearly demonstrated by classic examples: influenza and Respiratory Syncytial Virus (RSV) are archetypal winter illnesses, while chickenpox and measles often follow spring cycles tied to school years. Meanwhile, dengue fever surges during rainy seasons in Asia and Latin America, and norovirus, a highly contagious gastrointestinal illness, spreads efficiently through crowded indoor settings like cruise ships and care facilities during winter.
From Reaction to Proactive Intervention
The inherent predictability of these epidemiology cycles empowers public health to move from a historically reactive stance to a strategically proactive one. Modern forecasting and surveillance are at the heart of this transformation, integrating historical outbreak data, sophisticated climate models, and real-time surveillance to create a comprehensive picture of disease risk. Advanced mathematical and agent-based models can simulate disease spread by factoring in variables like temperature, humidity, and human mobility patterns. Concurrently, the field of digital epidemiology has emerged as a powerful tool, utilizing novel data sources such as wastewater testing, genomic sequencing of pathogens, and even anonymized social media data to provide early warnings of impending outbreaks or detect anomalies in established cycles. This data-driven approach allows public health systems to anticipate threats and allocate resources more efficiently, preparing for a surge before it arrives.
This enhanced predictive power has allowed for the implementation of precisely timed and highly effective interventions. For example, vaccination campaigns for influenza were scheduled for the fall to ensure that populations achieved peak immunity just before the traditional winter surge began. Similarly, vector control programs, including the spraying of insecticides and the elimination of standing water, were ramped up just before the onset of rainy seasons to suppress mosquito populations before they could multiply. These large-scale public health efforts were complemented by encouraging individual behaviors, such as consistent handwashing and the use of insect repellents, which helped disrupt transmission at the personal level. The ongoing challenges of climate change and rapid urbanization, which threatened to alter these predictable cycles, necessitated a vigilant and adaptive approach, where surveillance and response strategies were continuously refined to account for evolving global dynamics.