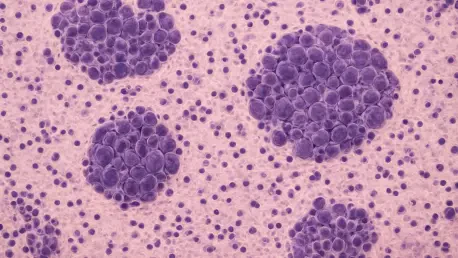
In a groundbreaking examination spanning over two decades, a comprehensive study conducted from 2000 to 2021 has unveiled critical insights into the landscape of neuroblastoma among children in Spain, focusing on those under 15 years of age. This pediatric cancer, recognized as the most common extracranial solid tumor in young patients, originates from neural crest cells of the sympathetic nervous system and presents a spectrum of outcomes—from spontaneous regression to aggressive, treatment-resistant forms. Analyzing a robust cohort of 1,774 cases sourced from national registries, the research highlights a compelling duality: a consistent incidence rate juxtaposed with remarkable strides in survival. Within Spain’s advanced healthcare framework, these findings not only reflect the nation’s progress in managing a complex disease but also spotlight persistent challenges that continue to shape the fight against childhood cancer. This narrative of steady prevalence paired with evolving clinical success sets a powerful stage for deeper exploration into how far the journey has come and where it must head next.
Unchanging Incidence: A Persistent Public Health Challenge
The incidence of neuroblastoma in Spain has remained strikingly stable over the 22-year study period, holding steady at 14.0 cases per million children aged 0–14. This rate aligns closely with patterns observed in other high-income nations, indicating that despite advancements in diagnostic technologies and broader access to healthcare, the frequency of this disease has not shifted significantly. Such consistency prompts critical questions about underlying factors—could biological mechanisms inherent to neuroblastoma be at play, or do systemic barriers hinder early identification? This unchanging prevalence underscores a public health burden that extends beyond mere treatment, calling for a deeper investigation into prevention and awareness strategies that might alter the trajectory of diagnosis rates in the years ahead.
Another concerning aspect tied to this stability is the lack of progress in the stage at which children are diagnosed. Over the two decades, the distribution of disease stages at the point of detection has shown little improvement, with many young patients still identified at advanced stages when treatment becomes far more complex and less effective. This stagnation points to gaps in early detection efforts, whether due to limited awareness among families and primary care providers or challenges in accessing specialized pediatric care. Addressing this issue requires not only technological innovation but also a concerted push to educate communities and streamline referral pathways to ensure that symptoms are recognized and acted upon sooner, potentially transforming outcomes for countless children.
Survival Improvements: Celebrating Clinical Breakthroughs
On a more hopeful note, survival rates for children diagnosed with neuroblastoma in Spain have shown substantial improvement over the study period, with the five-year overall survival rate rising from 74% in the early 2000s to an encouraging 81% by 2017. This upward trend is largely attributed to significant clinical advancements, including the adoption of targeted therapies such as anti-GD2 immunotherapy, which has proven transformative for many patients. Additionally, the integration of clinical trials, like the LINES trial, into standard care protocols has allowed for cutting-edge treatments to reach those with locoregional tumors, markedly enhancing their prognosis. These developments reflect a dynamic shift in pediatric oncology, showcasing how innovation can directly translate into lives saved.
Yet, the benefits of these advancements are not distributed evenly across all affected children. Disparities in survival outcomes persist, influenced by factors such as sex, age at diagnosis, tumor morphology, primary site, and disease stage. Notably, males and those with less advanced tumors have experienced greater gains, revealing an uneven landscape of progress. These differences highlight the necessity for more personalized treatment approaches that account for individual patient characteristics and ensure equitable access to the latest therapies. Bridging these gaps remains a critical priority, as the ultimate goal is to extend the benefits of modern medicine to every child battling neuroblastoma, regardless of their specific circumstances or clinical profile.
Data-Driven Insights: The Role of Cancer Registries
A pivotal element of the study’s success lies in the meticulous use of cancer registries, such as the Spanish Registry of Childhood Tumors and the Neuroblastoma Clinical Database, which have provided a comprehensive foundation for tracking disease trends. By merging population-based data with detailed clinical records, these systems minimize underreporting and offer a clearer picture of neuroblastoma’s impact across Spain. The adherence to stage-specific data collection guidelines has further enhanced the ability to monitor how the disease progresses and responds to interventions over time. This robust framework not only supports precise epidemiological analysis but also serves as a blueprint for other nations aiming to strengthen their own cancer surveillance efforts.
Beyond mere data collection, the practical implications of these registries are profound for shaping healthcare policy and patient care strategies. Detailed insights into who is diagnosed, at what stage, and with what outcomes enable targeted interventions that address specific needs within the population. For instance, identifying regions or demographics with higher rates of late-stage diagnoses can guide resource allocation and awareness campaigns. Spain’s model demonstrates how systematic data can bridge the gap between research findings and real-world impact, offering a valuable lesson for global health systems. As other countries look to improve their approaches to pediatric cancer, adopting similar registry practices could be a game-changer in understanding and combating diseases like neuroblastoma on a broader scale.
Looking Ahead: Addressing Gaps and Building on Success
Reflecting on the past 22 years, the journey of managing neuroblastoma in Spain reveals both remarkable achievements and areas demanding further attention. The steady incidence rate of 14.0 cases per million children stands as a reminder of an enduring challenge, while the rise in five-year survival from 74% to 81% marks a triumph of clinical innovation through therapies like anti-GD2 immunotherapy. However, the unchanged distribution of disease stages at diagnosis and persistent disparities in outcomes based on demographic and clinical factors paint a picture of incomplete progress that needs resolution.
Moving forward, the focus should shift to actionable strategies that tackle these lingering issues head-on. Enhancing early detection through widespread education for families and healthcare providers could shift more diagnoses to earlier, more treatable stages. Simultaneously, research must prioritize personalized treatments to close survival gaps across different patient groups. Strengthening global collaboration to share data and best practices from Spain’s registry model could further amplify impact. These steps, grounded in the lessons of the past, offer a roadmap to ensure that every child facing neuroblastoma receives the chance for a healthier future.