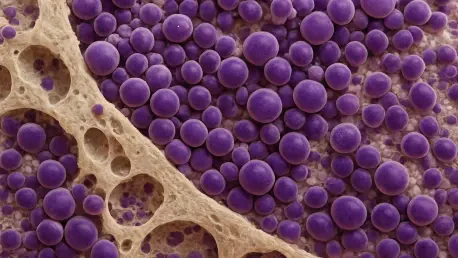
In a striking advancement for cancer care, a recent study from the University of York has revealed that survival rates for multiple myeloma, a prevalent type of blood cancer, have nearly doubled since 2005, marking a significant milestone in oncology. This research, published during Blood Cancer Awareness Month, underscores the transformative impact of medical innovation on patient outcomes. Analyzing data from over 3,700 individuals in England, the findings highlight how far treatment options have evolved, offering renewed hope to thousands diagnosed with this challenging disease each year. Multiple myeloma affects approximately 6,300 people annually in the UK, targeting plasma cells in the bone marrow and historically carrying a grim prognosis due to its aggressive nature. Yet, the landscape of care has shifted dramatically over the past two decades, driven by groundbreaking therapies and collaborative research efforts that continue to redefine what’s possible for patients facing this condition.
Unveiling Dramatic Survival Improvements
The centerpiece of this study is a remarkable statistic: median survival for myeloma patients has surged from 2.4 years in 2005 to 4.5 years in 2019, representing a near doubling of life expectancy. This leap forward is largely attributed to the advent of innovative treatments like bortezomib, a targeted therapy that stands in stark contrast to traditional chemotherapy. Unlike older approaches that often brought debilitating side effects, bortezomib offers a more effective and less toxic alternative, making it suitable for a diverse range of patients. This shift has fundamentally changed the way the disease is managed, allowing individuals to maintain a better quality of life while extending their time with loved ones. The data, drawn from real-world evidence in England, paints a clear picture of progress that transcends theoretical promise and delivers tangible results for those battling this blood cancer.
Beyond the raw numbers, this improvement in survival reflects a broader evolution in medical practice. The ability to tailor treatments to individual needs has been a game-changer, particularly for those who previously faced limited options due to the harshness of conventional therapies. The study’s findings emphasize that the introduction of gentler, more precise drugs has not only extended lifespans but also reduced the physical burden of treatment. Moreover, the increased survival time provides critical opportunities for patients to engage in meaningful moments, underscoring the human impact of these advancements. As researchers continue to build on this foundation, the focus remains on ensuring that such therapies become widely accessible, breaking down barriers that might prevent patients from benefiting from the latest breakthroughs in care.
Remarkable Gains for Older Patients
One of the most compelling aspects of the research is the unprecedented progress seen among older myeloma patients, particularly those aged 80 and above. The study reports a five-fold increase in five-year survival rates for this demographic since 2005, a statistic that highlights a significant shift in how care is delivered to vulnerable populations. Historically, older individuals were often excluded from clinical trials and aggressive treatments due to concerns about their ability to tolerate them. However, the emergence of less toxic therapies has paved the way for their inclusion, enabling this group to access cutting-edge options that were once out of reach. This change represents a profound step toward more inclusive healthcare, ensuring that age does not dictate the quality of treatment received.
Equally noteworthy is the role that clinical trial participation has played in driving these outcomes for older patients. The data indicates that greater involvement in research studies has allowed for therapies to be tested and adapted to meet the specific needs of this age group. This trend challenges long-standing assumptions about frailty and treatment eligibility, demonstrating that tailored approaches can yield extraordinary results even in advanced age. The success among those over 80 serves as a powerful reminder that medical innovation must prioritize all segments of the population. As the field moves forward, sustaining this momentum will require ongoing efforts to expand trial access and refine therapies, ensuring that the benefits of progress are felt across every age bracket without exception.
The Power of Research and Teamwork
At the heart of these survival gains lies a robust framework of research and collaboration, exemplified by the University of York’s Centre for Blood Research and its partnership with the Haematological Malignancy Research Network (HMRN). This alliance, involving NHS clinicians, has leveraged detailed, real-world datasets to uncover critical insights into blood cancers like myeloma. Such collaborative efforts have been instrumental in translating scientific discoveries into practical solutions that directly improve patient outcomes. Experts from various organizations, including Cancer Research UK and Blood Cancer UK, consistently highlight that clinical trials and data-driven innovation are the cornerstones of this progress, shaping a future where survival continues to improve through evidence-based advancements.
Furthermore, the synergy between academic institutions and healthcare systems illustrates the importance of a unified approach to tackling complex diseases. The HMRN’s unique ability to collect high-quality data provides a foundation for addressing pressing questions about treatment efficacy and long-term trends. This collaborative model not only accelerates the development of new therapies but also informs health policy, ensuring that systemic changes align with patient needs. Voices from the field stress that continued investment in research infrastructure is vital to maintaining this trajectory. By fostering environments where data and expertise converge, the medical community can push boundaries further, turning incremental gains into lasting victories for those affected by myeloma and beyond.
Navigating Persistent Obstacles
Despite the impressive strides in survival, challenges remain that temper the celebration of these achievements. Survival rates for myeloma, while improved, still fall short compared to many other cancers, signaling a pressing need for sustained focus and resources. Systemic issues, such as limited access to clinical trials for certain patient groups and delays in integrating novel treatments into standard care, pose significant hurdles. These barriers can prevent timely delivery of life-extending therapies, leaving some individuals without the benefits of recent innovations. Addressing these gaps requires a concerted effort to streamline processes within healthcare systems like the NHS, ensuring that breakthroughs reach patients swiftly and efficiently.
Additionally, the disparity in outcomes underscores the importance of identifying and dismantling obstacles that hinder progress. Advocacy for increased funding is a recurring theme among experts who argue that financial support is crucial for driving research and expanding trial opportunities. The complexity of myeloma demands ongoing innovation to develop even more effective treatments with fewer side effects. Beyond funding, there’s a call for policies that prioritize rapid adoption of new therapies, minimizing bureaucratic delays that can impact patient care. As the medical field grapples with these issues, the focus remains on creating a healthcare landscape where every patient, regardless of circumstances, can access the full spectrum of available advancements without unnecessary setbacks.
Building a More Inclusive Future
The research also sheds light on a growing movement toward health equity in cancer care, with older patients experiencing some of the most significant survival improvements in recent years. This trend reflects a broader commitment to ensuring that medical advancements benefit all demographics, challenging past practices that often overlooked certain groups. However, achieving true equity remains an evolving goal, as access to clinical trials and cutting-edge treatments is not yet uniform across all populations. Factors such as socioeconomic status, geographic location, and background continue to influence who can participate in research or receive the latest therapies, highlighting the need for systemic reforms to level the playing field.
Moreover, stakeholders emphasize that breaking down these barriers is essential to sustaining the momentum of survival gains. Efforts to expand trial availability and tailor outreach to underrepresented groups are critical steps in this direction. The success seen among older patients serves as a blueprint for what’s possible when inclusivity is prioritized, but it also reveals how much work remains to ensure similar outcomes for others. The call for a stronger NHS framework, one that embeds research and equity into its core, resonates as a pathway forward. By aligning resources and policies with the goal of universal access, the fight against myeloma can continue to evolve, offering hope that future advancements will reach every corner of society without distinction or delay.
Reflecting on Milestones and Next Steps
Looking back, the University of York’s study marked a pivotal moment in the journey against multiple myeloma, with median survival nearly doubling over a span of 14 years. The impact of targeted therapies and inclusive clinical trials reshaped the prognosis for countless patients, especially those in older age groups who once faced limited options. Collaborative research, underpinned by real-world data, proved to be the catalyst for these life-changing outcomes. Yet, the persistent gap in survival rates compared to other cancers served as a stark reminder that the battle was far from over. Moving forward, the focus must shift to actionable strategies—bolstering funding, enhancing trial access, and accelerating therapy integration within healthcare systems. The upcoming National Cancer Plan for England presents a vital opportunity to embed these priorities, ensuring that past achievements become the foundation for even greater progress in the years ahead.