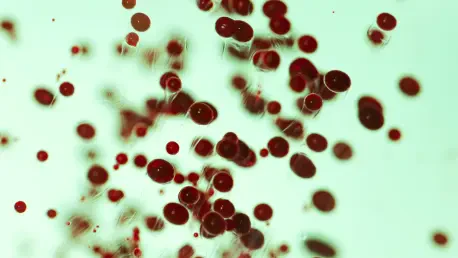
A recent comprehensive investigation by the Centers for Disease Control and Prevention (CDC) has brought a critical public health challenge into sharp focus, identifying extraintestinal invasive Escherichia coli as the foremost cause of sepsis that begins outside of a hospital setting. This landmark surveillance study was initiated to address a significant void in public health data, aiming to meticulously characterize the pathogen’s epidemiology, map its dominant strains, and quantify the alarming spread of its resistance to essential antibiotics. Before this initiative, led by Dr. Heather Grome of the CDC’s Division of Healthcare Quality Promotion, no routine surveillance existed for invasive E. coli in the United States, despite its severe clinical impact and the known potential for its genetic resistance mechanisms to transfer to other dangerous bacteria. The research sought to build a foundational understanding necessary for developing effective prevention strategies and improving the clinical detection of this life-threatening condition that silently escalates from common infections.
A Comprehensive Surveillance Effort
The investigation was a robust, multi-faceted surveillance study combining laboratory analysis with population-based tracking, conducted under the established frameworks of the CDC’s Emerging Infections Program (EIP) and the Multi-site Gram-negative Surveillance Initiative (MuGSI). The scope of the project was substantial, encompassing a diverse population of over 7.2 million people residing in selected metropolitan counties across nine different EIP sites, including California, Colorado, Georgia, Maryland, Minnesota, New Mexico, New York, Oregon, and Tennessee. Data for this intensive study were meticulously gathered and analyzed over a concentrated three-month period from June to August of 2023, providing a detailed snapshot of the pathogen’s prevalence and characteristics within these communities. This broad and systematic approach was designed to capture a representative sample of cases to accurately estimate the national burden of the disease and identify overarching trends in its transmission and clinical presentation across different demographic and geographic areas.
The study employed a precise definition for an “incident case,” which was categorized as the first isolation of E. coli from a normally sterile body site, such as the bloodstream or cerebrospinal fluid, regardless of the bacterium’s antimicrobial susceptibility profile. Upon initial identification of potential cases through automated queries of clinical laboratory testing systems, each one underwent a thorough and detailed medical record review. This critical secondary step allowed investigators to ascertain a wealth of comprehensive information, including patient demographics, significant underlying medical conditions, previous healthcare exposures, ultimate clinical outcomes, the specific type of infection associated with the invasion (such as a urinary tract infection), and the complete results from antimicrobial susceptibility tests. Through this rigorous process, the team identified 1,345 distinct cases of invasive E. coli infection among 1,334 unique patients. The data revealed that the vast majority of these infections, 1,223 cases or 90.9%, were bacteremia, with the pathogen isolated from blood, while the urinary tract was pinpointed as the most frequent initial source of these dangerous systemic infections.
Unveiling a Significant Public Health Burden
The collected data painted a concerning picture of the widespread burden of invasive E. coli, corresponding to an estimated annual incidence of 74.7 cases for every 100,000 people in the population. The study’s findings confirmed a disproportionate impact on specific demographic groups, with older adults aged 60 and over, as well as women, experiencing significantly higher rates of infection. The clinical severity associated with these cases was stark and undeniable. An overwhelming 95.1% of the case-patients, totaling 1,279 individuals, required hospitalization to manage their condition, placing a substantial strain on healthcare resources. Furthermore, the mortality rate was significant, as 106 patients, or 7.9% of the total cohort, ultimately died as a direct result of the infection. These statistics powerfully underscore the serious and often fatal threat that invasive E. coli poses to communities, moving it far beyond the perception of a simple or easily managed pathogen and establishing it as a major public health priority demanding immediate and focused attention from clinicians and policymakers alike.
One of the most alarming consensus viewpoints to emerge from the surveillance data was the widespread and deeply troubling level of antimicrobial resistance observed among the E. coli isolates. Resistance to two commonly prescribed frontline antibiotics was highly prevalent; 25.9% of the isolates tested were found to be resistant to ciprofloxacin, and an even higher 28.8% were resistant to trimethoprim-sulfamethoxazole. Perhaps the most concerning discovery of all was that nearly 14% of all infections (specifically 13.8%, or 185 cases) were caused by extended-spectrum ß-lactamase-producing (ESBL) E. coli strains. These ESBL-producing organisms are notoriously difficult to treat, as they are resistant to many powerful penicillin and cephalosporin antibiotics, which are often the go-to agents for serious infections. The authors of the study characterized this high prevalence as “alarming,” suggesting that the rise of ESBL E. coli should compel clinicians to fundamentally reconsider their empiric treatment choices for common syndromes like urosepsis, where E. coli is the most frequently expected pathogen and delayed effective therapy can have devastating consequences.
A Potential Path Toward Prevention
The surveillance effort successfully identified a clear dominance of specific O-antigen serotypes, a finding that provided a direct and actionable pathway for developing preventative public health measures. The three most prevalent serotypes identified were O25B, which was found in 16.2% of all isolates, followed by O2 at 11.0% and O6 at 9.9%. This serotype distribution was consistent with findings from other global research and lent strong support to the ongoing clinical trials for several polysaccharide conjugate vaccine candidates. These promising vaccines were specifically designed to target these common and highly invasive O antigens. The investigators posited that the development and successful deployment of an effective vaccine against invasive E. coli could be a transformative event in public health. Such a vaccine would not only have directly reduced the significant burden of invasive disease and its associated morbidity and mortality but would also have played a crucial role in a broader, long-term strategy to mitigate the growing crisis of antimicrobial resistance by preventing infections from occurring in the first place, thereby decreasing the overall reliance on and use of antibiotic treatments.