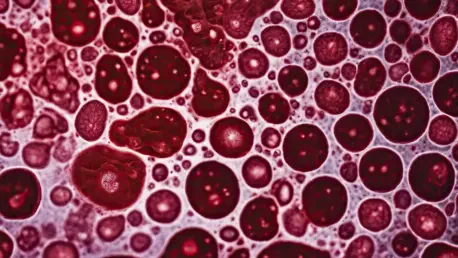
The landscape of medical treatment for blood cancer patients is witnessing a transformative shift, thanks to innovative research on blood stem cell transplants. This research particularly delves into the safety and efficacy of “mismatched” transplants, a domain that has historically posed significant risks. For patients suffering from blood cancers such as leukemia, lymphoma, or myelodysplastic syndrome, finding a perfectly matched donor has always been the aspirational goal, yet often unattainable. The promising clinical trial from the UVA Cancer Center introduces cyclophosphamide as a game-changer in reducing graft-versus-host disease, an immune response that has deterred mismatched transplant feasibility.
Revolutionary Treatment Approach
Cyclophosphamide’s Role and Advantages
Mismatched transplants traditionally carry a high risk of graft-versus-host disease, causing the recipient’s immune system to attack the foreign cells introduced through the transplant. The introduction of cyclophosphamide marks a significant shift in this paradigm. This drug’s efficacy in preventing the majority of adverse reactions associated with mismatched transplants paves the way for broader applications and more inclusive treatment options. Key findings from the UVA study highlight that a remarkable 80% of patients administered cyclophosphamide were alive after one year, exhibiting a success rate on par with fully matched transplant recipients. Furthermore, only 10% of these patients developed moderate to severe or chronic graft-versus-host disease, showcasing outcomes comparable to traditional transplant methods. The implications of these outcomes are profound, opening doors to effective treatment for patients previously marginalized due to the absence of a perfectly matched donor.
Access to Diverse Donor Pools
This breakthrough expands treatment possibilities significantly, offering new hope to patients across diverse backgrounds. Historically, racial and ethnic minorities often faced limited donor options, a barrier that hampered access to life-saving procedures. With the advent of cyclophosphamide-enhanced mismatched transplants, these patients can now find compatible donors more efficiently, elevating their chances for successful transplants. The UVA study outlines how all eligible patients secured suitably matched donors, highlighting a dramatic shift in donor availability. The research carried out by UVA Health underscores the importance of this advancement, catalyzing a critical change in the accessibility of blood stem cell transplants to wider demographic sections. This milestone achievement sets a promising precedent for the medical community, propelling efforts to create equitable healthcare solutions.
Groundbreaking Clinical Outcomes
Robust Research Backing
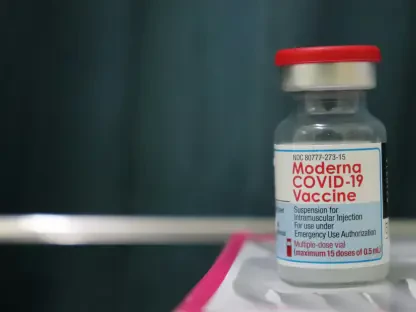
The cyclophosphamide study is not merely an isolated discovery. The research is published in The Journal of Clinical Oncology, underscoring its significance within the scientific community and validating its findings through esteemed support from the National Institutes of Health, among others. This robust endorsement amplifies the credibility of cyclophosphamide as a viable option for facilitating safer, mismatched blood stem cell transplants. It demonstrates a shared commitment within the scientific realm to revolutionize treatment approaches. The empirical data amassed from the study propels the argument forward that cyclophosphamide could redefine current treatment protocols, making previously inaccessible transplants a reachable reality for many suffering from blood cancers.
Clinical Implications and Future Directions
As the research community absorbs these insights, a tantalizing question arises about the future directions cyclophosphamide might inspire. Its efficacy suggests potential applications beyond the transplant setting, encompassing wider oncological interventions. Moving forward, investigators may explore augmented protocols or integrated therapies that leverage cyclophosphamide’s immune-modulating properties while refining its administration. Such advancements could usher in new paradigms in cancer treatment, expanding horizons even within cellular therapies that synergize with other immunological strategies. The promising outcomes from ongoing trials might further catalyze regulatory changes, expediting the adoption of cyclophosphamide therapy in clinical norms—potentially influencing global healthcare systems swiftly.
The Impact on Patients and Medical Practices
Transformative Effects on Patient Care
The extraordinary advancement signifies a transformative era for blood cancer patient care, broadening treatment accessibility and offering renewed hope to countless individuals. The ability to accommodate mismatched donors minimizes barriers that previously impeded medical intervention, providing timely solutions to a pressing healthcare challenge. This evolution in treatment protocols may also alter patient experiences fundamentally, alleviating the once-overpowering fear of adverse post-transplant reactions. Cyclophosphamide holds the promise of significantly lowering such risks and improving quality of life in the aftermath of transplants, contributing to holistic recovery pathways.
The Future of Transplant Medicine
The landscape of medical treatment for blood cancer patients is undergoing a significant transformation, driven by innovative breakthroughs in blood stem cell transplants. This cutting-edge research focuses on the safety and effectiveness of “mismatched” transplants, a field historically fraught with considerable risks. Patients battling blood cancers like leukemia, lymphoma, or myelodysplastic syndrome have traditionally faced challenges in securing a perfectly matched donor, an ideal often out of reach. However, promising developments from the UVA Cancer Center’s clinical trial suggest a paradigm shift. Introducing cyclophosphamide has emerged as a pivotal advancement in mitigating graft-versus-host disease, an adverse immune response that has long inhibited mismatched transplant applications. This emerging strategy not only broadens treatment options but also enhances the prospects for patients who previously had limited access to lifesaving procedures, signifying a hopeful horizon for blood cancer therapies.