The mental health care system within U.S. Army Special Forces, also known as Green Berets, is facing significant challenges. These elite soldiers, who endure numerous combat deployments, are often reluctant to seek help due to cultural and structural barriers. The tragic suicide of Master Sgt. Matthew Livelsberger highlights the broader issues within Special Forces mental health care.
Systemic Flaws and Cultural Reluctance
Reluctance to Seek Help
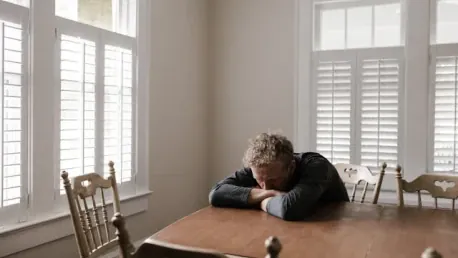
Special Forces troops often avoid seeking mental health care due to fears of being removed from their units or stigmatized. The culture within these elite units prioritizes continuous deployment and toughness, fostering an environment where soldiers hide their mental health issues. A prevalent belief that seeking help could signify weakness reinforces this reluctance, making soldiers hesitant to address and acknowledge their mental health concerns openly. This cultural environment creates significant barriers to receiving care, leaving many soldiers to suffer in silence.
The intensity of the operational commitments expected of Special Forces means that mental health issues are often masked to maintain readiness. Soldiers prefer to downplay their problems rather than risk their positions or future assignments within their units. This inevitably leads to untreated mental health issues, as acknowledging them might result in adverse career consequences. Consequently, the reluctance to seek help not only harms individual soldiers but also jeopardizes unit effectiveness, creating a vicious cycle of deteriorating mental health within the force.
Impact of Continuous Deployments
The relentless operational tempo associated with the War on Terror has exacerbated mental health problems among Special Forces. Soldiers frequently undergo numerous deployments within a short period, significantly impacting their mental well-being and leaving little room for recovery. This continuous deployment cycle results in prolonged exposure to combat stress and trauma, which in turn increases the risk of developing mental health disorders such as PTSD, depression, and anxiety.
For Special Forces, the expectation to be continually battle-ready allows minimal time for mental decompression. The constant state of alertness and exposure to danger during deployments accumulates mental strain. Soldiers often transition directly from one combat zone to another with inadequate recovery periods, intensifying their psychological burdens. This lack of sufficient downtime between deployments discourages mental health recuperation, further ingraining the significant impacts on soldiers’ overall well-being and functionality.
Command Influence and Pressure
Manipulation of Mental Health Programs
Special Forces Group commanders often pressure embedded mental health professionals to downplay conditions to keep soldiers operational. This manipulation includes ignoring excessive alcohol consumption or altering medication to ensure troops can remain in the field. Such command interference compromises the objectivity and effectiveness of mental health care, as medical professionals are compelled to make decisions based on operational priorities rather than clinical needs.
Commanders, aiming to maintain a ready force, may sometimes push mental health professionals to declare soldiers fit for duty, even when their condition necessitates a break from operational responsibilities. This manipulation of mental health care undermines the integrity of medical evaluations and compromises the welfare of soldiers. By prioritizing deployment readiness over mental well-being, the systemic health care setup fails to provide adequate support for those who need it most.
Lack of Proper Oversight
Mental health care within Special Forces lacks proper oversight. The pressures and expectations placed on embedded mental health professionals undermine their ability to provide effective care, resulting in untreated or inadequately treated issues. The dual role of embedded professionals, responsible for both providing care and maintaining operational readiness, complicates their position. The military hierarchy places undue influence on these professionals, who may feel obligated to conform to command directives rather than adhering strictly to medical protocols.
The lack of independent oversight allows the manipulation of mental health programs to persist unchallenged. Without external accountability, embedded mental health providers operate within a constrained environment, unable to challenge or report command interference effectively. This structural flaw means that many soldiers do not receive the comprehensive care they require, leading to a mental health support system that fails to serve its intended purpose adequately.
High Suicide Rates
Alarming Statistics
Reports indicate higher suicide rates among Special Forces compared to general armed forces and civilian populations. A Defense Suicide Prevention Office report revealed that suicide deaths among Army Special Operations Command troops surged from six in 2017 to 18 in 2022. These statistics reflect a disturbing trend, underscoring significant mental health care deficiencies within these elite units. The elevated suicide rate serves as a stark reminder of the urgency to address mental health care failures and the dire consequences of inaction.
The heightened suicide rates point to systemic issues that transcend individual circumstances. Factors such as the relentless operational tempo, cultural stigmatization, and command interference in mental health support collectively contribute to this crisis. These alarming numbers necessitate an immediate evaluation and overhaul of current mental health care practices to prevent further loss of life and ensure soldiers receive the necessary support to cope with their unique challenges.
Case Studies
The suicides of Master Sgt. Matthew Livelsberger and movie star turned soldier Staff Sgt. Mike Mantenuto illustrate the profound impacts of mental health care deficiencies. Both cases emphasize failures in the mental health care system and the harmful consequences of not addressing soldiers’ needs properly. Livelsberger’s suicide, which occurred in a dramatic public display, shocked the community and underscored the pressing need for comprehensive mental health reform within Special Forces. Despite showing clear signs of mental distress, he did not receive the necessary interventions, reflecting the systemic issues at play.
Mantenuto’s tragic death similarly highlights the paradox within the current mental health framework. Despite being entrusted with leading a peer-support group, Mantenuto grappled with his own mental health struggles, which ultimately went unaddressed. His case demonstrates the lack of robust support mechanisms and the consequences of neglecting mental health care, even among those tasked with providing peer assistance. These poignant examples illustrate the dire need for a reformed approach that genuinely prioritizes soldiers’ mental well-being above operational mandates.
Mental Health Program Manipulation
Embedded Mental Health Programs
Embedded mental health programs within Special Forces, initially intended to offer specialized support, have been compromised by commanders. This manipulation leads to mistrust and inadequate care for troops suffering from mental health and substance abuse issues. When mental health professionals are pressured to prioritize operational needs over clinical evaluations, the integrity of care provided is severely compromised. Soldiers quickly become aware of this dynamic and may feel discouraged from seeking help, knowing that their issues might not be addressed appropriately.
The original intention behind embedded mental health programs was to offer accessible, on-the-ground support tailored to the unique stressors faced by Special Forces. However, the interference by command structures has corrupted this vision, creating a system where soldiers cannot trust that their mental health concerns will be handled impartially and professionally. This erosion of trust undermines the effectiveness of these programs, leaving soldiers without reliable mental health resources.
Consequences of Manipulation
The manipulation of mental health programs by commanders results in a cycle where troops avoid seeking help due to stigma and fear of repercussions. This ultimately leads to increased rates of suicide and untreated mental health problems. Soldiers, perceiving that their mental health concerns will not be taken seriously or managed confidentially, may resort to self-destructive coping mechanisms, further exacerbating their struggles. This situation perpetuates the cycle of untreated mental health issues and deteriorating well-being within the Special Forces community.
The broader implications of this manipulation extend beyond individual soldiers, affecting unit cohesion and operational effectiveness. When soldiers cannot seek or receive adequate mental health care, the overall readiness and resilience of the force are compromised. Addressing this systemic issue requires a fundamental overhaul of the current approach, ensuring that mental health programs operate with full professional autonomy and are free from command interference.
Need for Systemic Reforms
Reducing Mission Pressures
Calls for reform focus on reducing mission pressures on forces dealing with mental health issues. This includes modifying operational demands to prevent overburdening soldiers and allowing sufficient recovery time between deployments. A strategic review of deployment schedules and mission assignments is necessary to ensure that soldiers are not continuously exposed to high-stress combat environments without adequate periods of rest and mental recuperation.
By prioritizing soldiers’ mental health alongside operational readiness, reforms can create a more supportive environment that values the well-being of personnel. Implementing policies that balance mission requirements with mental health needs can help alleviate the relentless pressure that currently exacerbates mental health conditions within Special Forces. This approach not only addresses individual well-being but also enhances overall unit performance and sustainability.
Ensuring Independent Oversight
Ensuring independent oversight of mental health services is crucial to avoid commander manipulation. This would help restore trust in the mental health care system and ensure that soldiers receive the care they need without fear of repercussions. Independent oversight bodies can provide impartial evaluations, ensuring that mental health care decisions are based solely on clinical assessments rather than operational expediencies. This system protects the integrity of mental health support and fosters an environment where soldiers feel safe to seek help.
Establishing clear boundaries between operational command and mental health care services is vital for creating a trustworthy and effective support system. Independent oversight can monitor and enforce these boundaries, making sure that mental health professionals can carry out their duties without external pressures. This reform is essential for rebuilding confidence in the mental health care system and ensuring that it effectively addresses the unique challenges faced by Special Forces soldiers.
Cohesive Narrative and Detailed Findings
Pressure on Troops
Special Forces soldiers frequently deploy, facing intense combat situations that contribute to significant mental health burdens. The relentless operational demands do not allow sufficient recovery time between deployments, exacerbating the mental stress. Combat experiences are inherently intense and can leave lasting psychological scars, but the pressures faced by Special Forces are magnified by the frequency and duration of their missions. This constant exposure to high-stress environments takes a severe toll on their mental well-being.
The high operational tempo leaves little room for mental health stabilization, creating an environment where soldiers are always on the brink of their psychological limits. Effective mental health support must consider the cumulative impact of these repeated stress exposures and provide adequate recovery periods. Without such considerations, the mental resilience of soldiers continues to erode, underscoring the need for a balanced approach that accommodates both operational requirements and mental health necessities.
Cultural Stigma and Command Influence
A culture of toughness discourages soldiers from admitting mental health struggles. This stigmatization, combined with command pressure to minimize reported issues, results in many soldiers’ problems going untreated. Within the Special Forces community, there is an inherent expectation to demonstrate unwavering resilience, which often translates into a reluctance to seek mental health support. This cultural attitude, perpetuated by both peers and superiors, fosters an environment where admitting to mental health struggles is perceived as a sign of weakness.
Command influence further compounds this issue by prioritizing operational readiness over addressing mental health concerns. Mental health professionals embedded within units face significant pressure to declare soldiers fit for duty, even when clinical evaluations suggest otherwise. This dual pressure from cultural expectations and command directives creates a toxic environment where genuine mental health needs are frequently sidelined, leading to untreated conditions and exacerbated mental health challenges.
Increased Suicide Rates
Empirical data points to a worrying increase in suicides among Special Forces, highlighting the failure of current mental health support systems. This trend underscores the need for comprehensive reform in how mental health care is delivered and overseen. The significant rise in suicide rates among this elite group starkly illustrates the devastating consequences of inadequate mental health support. These statistics are not merely numbers but represent a tangible human cost that demands urgent and effective action.
The current mental health care system’s inability to address the unique challenges faced by Special Forces soldiers contributes directly to these alarming suicide rates. Comprehensive reform must prioritize creating a support system that can cater to the specific needs and pressures of these elite warriors. Addressing the underlying causes of mental health issues and providing robust, unbiased support structures can help reduce the suicide rates and improve overall mental well-being within the Special Forces community.
Case Study Insights
The mental health care system for U.S. Army Special Forces, known as the Green Berets, is currently grappling with significant problems. These elite soldiers, who undergo numerous and often grueling combat deployments, frequently hesitate to seek mental health assistance. This reluctance is largely due to a combination of cultural and structural barriers within the military.
One poignant example of the ongoing crisis is the tragic suicide of Master Sgt. Matthew Livelsberger. His death serves as a stark reminder of the underlying mental health issues and the inadequate support systems that exist for Special Forces soldiers. Despite their bravery and strength in the field, these soldiers face immense psychological struggles that are often left unaddressed.
The stigma associated with seeking help in a high-pressure, high-performance environment discourages many from reaching out. Additionally, there are institutional challenges, such as limited access to specialized mental health professionals and a lack of adequate follow-up care. For many Green Berets, the fear of appearing weak or jeopardizing their careers further exacerbates the problem.
Efforts to improve the mental health care system for these elite soldiers must focus on creating a culture that encourages seeking help, along with enhancing access to professional care. Comprehensive support systems are essential to address the unique challenges faced by Green Berets, ensuring that they receive the mental health care they need and deserve.