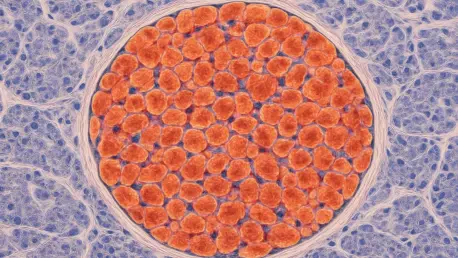
In a remarkable advancement for medical science, researchers at Scripps Research have identified a previously unknown type of cell in the pancreas that could revolutionize the approach to managing type 1 diabetes, a chronic condition affecting 1.6 million Americans, by offering new hope for prevention and treatment. Named vascular-associated fibroblastic cells (VAFs), these specialized cells serve as protectors of insulin-producing beta cells, safeguarding them from the immune system’s erroneous attacks that define this debilitating disease. The significance of this breakthrough lies not only in unveiling a new cellular player in pancreatic health but also in offering a potential pathway to prevent or even reverse the progression of type 1 diabetes. By understanding how VAFs maintain immune tolerance, scientists are now poised to explore innovative therapies that could reduce reliance on current treatments like insulin injections and harsh immunosuppressive drugs, paving the way for more targeted and effective solutions.
Unveiling a Hidden Guardian in the Pancreas
The discovery of VAFs marks a pivotal moment in understanding how the pancreas naturally defends itself against autoimmune threats. These cells operate as molecular mediators, presenting fragments of pancreatic tissue to immune cells while simultaneously signaling for tolerance—a process that prevents the immune system from misidentifying and attacking the body’s own insulin-producing beta cells. This protective mechanism helps explain the often-silent preclinical phase of type 1 diabetes, during which immune activity ramps up without immediate symptoms or detectable blood sugar abnormalities. By acting as gatekeepers, VAFs maintain a delicate balance that, when intact, keeps autoimmunity at bay. This finding shifts the focus from merely reacting to immune attacks to proactively supporting the body’s inherent safeguards, offering a fresh lens through which to view disease prevention.
Beyond their protective role, VAFs highlight the complexity of immune regulation within the pancreas, an organ uniquely vulnerable due to its role in digestion and constant exposure to external stressors. Research led by Professor Luc Teyton at Scripps Research utilized cutting-edge techniques, such as advanced imaging and specialized cell-labeling methods, to uncover how these cells interact with the immune system. However, persistent inflammation from factors like diet, environmental toxins, or infections can overwhelm VAFs, disrupting their ability to induce tolerance. When this happens, the immune system may turn hostile, targeting beta cells and triggering the onset of type 1 diabetes. Recognizing this vulnerability underscores the importance of early intervention to preserve VAF functionality before irreversible damage occurs, potentially changing the trajectory of the disease.
Rethinking Type 1 Diabetes Treatment Strategies
For millions grappling with type 1 diabetes, the daily reality of insulin injections, meticulous blood sugar monitoring, and the looming threat of complications like kidney failure or vision loss is a heavy burden. The emergence of VAFs as a key player in immune tolerance offers a glimmer of hope for more effective management strategies that address the root cause—autoimmune destruction—rather than just its consequences. Future therapies could aim to enhance the protective capabilities of VAFs, perhaps by boosting their ability to pacify immune cells or by developing anti-inflammatory treatments to shield them from stress. Such approaches might halt disease progression during its early, preclinical stages, preserving beta cell function and reducing the need for lifelong insulin dependence.
This discovery also prompts a broader rethinking of how type 1 diabetes is approached in clinical settings, moving away from broad-spectrum immunosuppression that often carries significant side effects. By focusing on bolstering the body’s natural tolerance mechanisms, as mediated by VAFs, medical research is trending toward personalized and less invasive interventions. The potential to intervene before full-blown symptoms emerge could transform lives, allowing individuals at risk to maintain normal pancreatic function for longer periods. While still in early stages, this shift in perspective aligns with a growing emphasis on precision medicine, where treatments are tailored to the specific biological processes at play in each patient, maximizing efficacy while minimizing harm.
Exploring Broader Medical Implications
The significance of VAFs extends far beyond the realm of type 1 diabetes, hinting at applications in other autoimmune disorders where immune tolerance is disrupted. Similar cellular mechanisms might exist in different tissues, suggesting that identifying and harnessing equivalent “peacekeeper” cells could lead to breakthroughs in conditions like rheumatoid arthritis or lupus. Additionally, the field of organ transplantation, where immune rejection remains a critical challenge, could benefit from strategies inspired by VAFs’ ability to prevent harmful immune responses. Researchers, including collaborators at Scripps Research, are eager to investigate these parallels, aiming to uncover universal principles of immune regulation that could inform a wide array of medical therapies.
Delving deeper into the role of VAFs also opens up questions about how environmental and genetic factors influence their function across diverse populations. If therapies can be developed to mimic or enhance VAF-mediated tolerance, the reliance on aggressive drugs that suppress the entire immune system might diminish, reducing risks of infections and other complications. The vision is to create targeted treatments that work in harmony with the body’s natural defenses, a goal that, while ambitious, is grounded in the tangible evidence provided by this discovery. As studies progress over the coming years, the hope is to translate these insights into practical solutions that address not just type 1 diabetes but a spectrum of immune-related challenges.
Navigating Challenges on the Road to Innovation
While the identification of VAFs sparks excitement, translating this scientific milestone into viable treatments presents substantial obstacles. The intricate nature of immune regulation means that a one-size-fits-all solution is unlikely; individual variations in inflammatory triggers and genetic predispositions complicate the development of universal therapies. Moreover, chronic inflammation, which undermines VAFs’ protective role, stems from diverse sources that are often difficult to control, ranging from lifestyle factors to unpredictable infections. Addressing these variables will require comprehensive clinical studies and innovative approaches to ensure that interventions are both safe and effective across different patient profiles.
Despite these hurdles, there is a palpable sense of cautious optimism among the scientific community about the potential of VAFs to reshape medical practice. The focus now shifts to actionable next steps, such as designing therapies that specifically target these cells’ tolerance-inducing functions without disrupting other immune activities. Collaborative efforts are underway to refine these strategies, balancing the promise of innovation with the practical realities of application. As research unfolds, the ultimate aim remains clear: to leverage this newfound understanding of pancreatic immunity to improve outcomes for those with type 1 diabetes and beyond, ensuring that hope translates into tangible progress.