It’s hard to believe that just four years ago we were in a global lockdown, relying on technology to order groceries, dial into work and school, and even connect with friends and family. Our idea of heroes became the everyday people on the frontline; nurses and doctors, factory workers and delivery drivers, and the artists who inspired us with balcony concerts. Against this backdrop of life interrupted, was life lost. And while millions have recovered from the virus, there are those dealing with the effects of long covid. While considerable effort to understand the symptoms and effect of long covid are underway, scientists still believe there’s a fair amount of mystery. Here’s where we are four years later.
Diagnosing Long Covid
The World Health Organization defines long covid as “the continuation or development of new symptoms three months after the initial SARS-CoV-2 infection, with these symptoms lasting for at least two months with no other explanation.” The fact that long covid presents differently in different people is part of what makes it difficult, with over 200 different symptom types linked to the infectious disease. Chief among these symptoms are brain fog, joint pain, fatigue, loss of taste and smell, and difficulty breathing.
Long covid, also called post-acute sequelae of SARS-CoV-2 (PASC) affects about 7% of Americans. While scientists and healthcare experts continue to look for treatment options, patients around the world continue to experience difficulties in their everyday lives, some, years after initially contracting the virus.
One of the factors contributing to the complexity of dealing with long covid is that it’s quite difficult to diagnose. Much like with covid, doctors have created a set of parameters to guide diagnosis. The majority of COVID-19 patients recover within a few weeks, at most, with some only experiencing symptoms for a few days. Doctors start considering a long covid diagnosis when symptoms are still present after four weeks. Through a process of elimination, healthcare workers are able to tell whether a patient has long covid, or is just experiencing a few lingering symptoms.
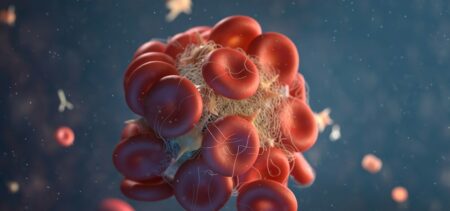
The discovery of blood biomarkers unique to long covid patients late last year was a breakthrough. According to experts, this means the development of diagnostic tests could be available sooner than initially thought.
Advanced research into long covid
To provide a definitive diagnosis and treatment cycle, advanced research into long covid is currently underway in a number of research institutes across the country. Notably, Mount Sinai, Stanford, and Yale have partnered with the government to roll out the RECOVER program. With some of the best experts in science and healthcare research, clinical trials are well underway, with studies trying to establish
- The number of Americans living with long covid
- The exhaustive list of symptoms related to long covid
- The effects in the body
- The impact on body tissue
- Treatment options
Scientists are determined to uncover new therapies that will radically improve, if not cure, long covid patients; their hope is embedded in the depth and breadth of clinical trials being conducted through the RECOVER program. 2024 is likely to be a year full of promise based on the available research data. Here are five predictions coming out of the clinical trials.
- Better identification and understanding of covid phenotypes
Thanks to the collaboration between healthcare professionals, scientists, caregivers, and patients, we can now identify four clinical groups that designate long covid:
- Chronic fatigue-like syndrome (includes symptoms like headaches and memory loss)
- Respiratory syndrome (characterized by coughing and shortness of breath/difficulties breathing)
- Chronic pain
- Neurosensorial syndrome (changes and/or loss of sense of taste and smell)
According to Dr Nisha Viswanathan, director of the long covid program at UCLA Health, the ability to accurately identify the specific clinical guidelines for each phenotype would result in better treatment for patients. Her hope is that 2024 sees the start of phenotype-specific treatment for her patients. “Many new medications are focused on different pathways of long COVID, and the challenge becomes which drug is the right drug for each treatment,” said Viswanathan.
- Monoclonal antibodies could be the answer
The emergence of monoclonal antibodies as a viable solution for the treatment and possible cure of long covid is something clinician-scientists will be delving into throughout 2024. Monoclonal antibodies, often synonymous with cancer treatment, are a targeted therapy. The antibodies are a result of cloning white blood cells that have a specific task; to locate and destroy the antigens associated with long covid.
In some smaller studies, this has already proved to be effective. The January 2024 edition of The American Journal of Emergency Medicine featured a case involving three patients who received the monoclonal antibodies and have shown complete recovery from long covid. “Remission occurred despite dissimilar histories, sex, age, and illness duration,” stated one of the authors.
Looking to replicate these results in a larger study, the University of California, San Francisco is leading a clinical trial to test targeted monoclonal antibodies. Dr David Patrino (PhD) leads the Mount Sinai Health System covid clinic in New York is hoping for similar results which “could be a game changer for a large swath of patients around the world. The idea is that the downstream damage caused by viral persistence will resolve itself once you wipe out the virus.”
- Could Paxlovid be the silver-bullet?
Paxlovid is a hybrid medication composed of two drugs, nirmatrelvir and ritonavir. Granted full approval from the Food and Drug Administration (FDA) in May 2023, Paxlovid treats mild to moderate COVID-19, specifically for patients identified as being at high risk for severe disease, hospitalization or death. Nirmatrelvir is an enzyme inhibitor, preventing viral replication, while ritonavir is an antiviral that helps increase the presence of antivirals in the body. Paxlovid is being tested by Dr Putrino’s team in a study aimed at post-viral patients who produce negative COVID-19 tests, but still experience the persisting symptoms of long covid.
Paxlovid differs from monoclonal antibodies in that it doesn’t just target the virus, it prevents replication. For patients that have yet to fully expel SARS-CoV-2, Paxlovid stands in the gap, potentially offering hope of a covid-free life.
While there’s tremendous potential for this drug to be the silver-bullet that solves long covid once and for all, critics have been vocal over the inconsistent results. While Paxlovid has eradicated long covid for some, it’s been completely ineffective for others. Naysayers have also been quick to point out the laundry list of side effects, including diarrhea, vomiting, nausea and further issues with the sense of smell. Under Dr Patrino, experts are hoping to answer the question of whether Paxlovid is indeed a silver-bullet treatment, and if not, who is best served by being administered this medication.
- Anti-inflammatories could provide another treatment path
Research indicates consistency in the inflammatory markers present in both patients with long covid and those with inflammation-related diseases like rheumatoid arthritis. This, according to a 2023 study published in the Journal of the American Medical Association.
Anti-inflammatories are a double-edged sword. On the one hand, clinicians are hopeful they’ll ease the inflammation that causes covid symptoms, allowing patients to experience relief. On the other hand, they can have serious side effects which include increased risk for infection, a burning skin sensation, and symptoms of the flu. According to Dr Grace McComsey, the physician leading the RECOVER program at University Hospitals Health System in Cleveland, the anti-inflammatories work by changing pathways in the immune system. Unfortunately, the levels of toxicity in medications raises questions around which drugs should be administered to which patients.
There are, of course, the less toxic alternatives, which were explored in a research piece published in The Lancet Infectious Diseases. Scientists discovered that metformin, used to treat diabetes, reduced the risk of developing long covid by up to 40%, when administered during the acute stage of a covid-positive patient. The benefits of using a drug like metformin is that it’s easily accessible and low in cost, with few side effects (in comparison to similar meds).
- Serotonin and long covid, could there be a link?
In November 2023, a study published in Cell provided incredible new research in our understanding of PASC and the factors contributing to viral persistence. It was discovered that patients with long covid consistently produced lower levels of serotonin than those not afflicted with the condition. In particular, popular antidepressant drug fluoxetine was able to improve the cognitive functioning of rats infected with the virus.
Key to the research findings is that serotonin reduction is in part due to an inability to absorb tryptophan; a naturally occurring amino acid connected to serotonin production. The next step in the research process is determining if increasing serotonin levels will improve symptoms of long covid patients.
Final Thoughts
While most of us have left covid behind, and even stopped using post-pandemic phrases like “the new normal”, for millions of people around the world COVID-19 is an ever-present affliction. Long covid, or PASC as it is referred to in the medical community, is the viral persistence caused by SARS-CoV-2. Patients experience symptoms for weeks, months, and even years after initial infection.
In an effort to better understand long covid, the RECOVER program was launched at research and medical institutions across the country. With large scale clinical trials taking place, RECOVER leans on the collaborative efforts of healthcare professionals, scientists, caregivers and patients, all in an effort to find solutions for the treatment of long covid.
2024, four years after the pandemic first torpedoed our lives, we are finally getting close to finding solutions. Four long covid phenotypes have been identified, with three different options being researched that could ultimately relieve the symptoms and destroy the antigens that perpetuate the viral persistence. 2024 could be the year we finally see the end of covid, for all.