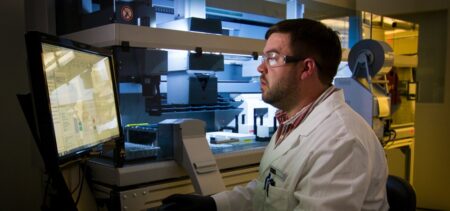
UnitedHealth has maintained that joining Optum and Change, two of the biggest providers of health IT services like revenue cycle management in the U.S., will result in a more connected administrative and payment ecosystem across healthcare. But after the deal was announced early last year, hospital and pharmacy groups swiftly came out against the merger, arguing it would result in fewer choices for services.
Hospital lobby the American Hospital Association also argued bringing Change under the umbrella of UnitedHealth, which also owns the biggest private payer in the country, UnitedHealthcare, could distort decisions about patient care, claims processing and denials at the expense of hospitals.