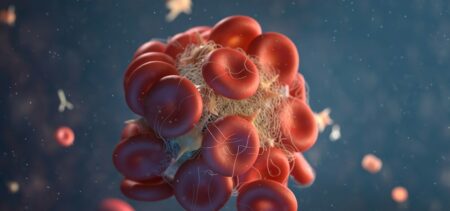
There is a certain standard procedure when patients come in with high blood pressure. Besides inquiring about lifestyle choices, doctors run specific tests. Depending on the test results, the possible most frequent causes are ruled out one by one. When these tests do not point out the cause of HBP, it might be the moment for a different approach. Studies indicated new hypertension and blood pressure genes that could play an important role in explaining this condition.
One of these studies comes from Queen Mary University of London. Although extremely interesting, a non-specialist might go through it and remain with one unanswered question. What is there to do when the reason for HPB is genetic?
What is there to do when the reason for HBP lies within the intricate genetic realm?
We’ll work our way towards the right answer to the above dilemma, if any at this moment. Nevertheless, correctly taking out of the question the other possible causes and determining that the cause is genetic helps when choosing the most suited drug therapies.
Why is that? Because otherwise the expectations could be creating false paths. Due to the fact that these patients do not positively respond to standard treatments, doctors will try different drug combinations. Going through countless types of medication might return the same unsatisfactory result.
Due to wrong therapeutic targeting, the doctors remain baffled, while the patient is not improving. Even more, blood pressure regulators come with side effects that might confuse things even more.
As one of the Queen Mary study authors, Patricia Munroe, says, revealing “new biological pathways through which the disease develops” can “also highlight potential new therapeutic targets”.
Standard risk factors and genetic predisposition to HBP
Any online source identifies the primary risk factors in high blood pressure. They correspond to the primary investigations performed by doctors on such patients. From family history, age, gender and race to behavior factors (diet, weight, life habits such as drinking or smoking), the risk factors all blur out in the mysterious “stress” causality.
Yet, at a closer look, the identity factors all have to do with genes: family history, age, gender and race are merely external manifestations of genes. Again, stress in in fact a personal reaction to stressful situations. Some cope in a better way, others develop mild or severe affections. Some may even die from prolonged stress. In extremely simple terms, certain individuals are wired to stand stressful situations better than others. Such an allegation covers countless of chemical and metabolic processes taking place inside an organism when exposed to certain stimuli.
It may just work to refrain from bad habits. Taking out of the equation a high-sodium diet, trying to lose weight or introducing physical activity in sedentary individuals could just work miracles. Nevertheless, we considered those cases where such changes seem to show no effect. After a while, doctors just shrug and point to stress as being the only culprit still available.
*Of course, there are cases where doctors suspect patients are not being honest about really changing their unhealthy habits. Truth be told, this may happen in many cases, too. As a nugget of wisdom, it would be less confusing to honestly report any progress or latency in improving your lifestyle to your physician.
When high blood pressure has no identifiable cause, doctors refer to it as primary hypertension.
While studies benefit professionals, patients should also take them into account
A 2011 study underlined the same link between genes and high blood pressure. Professionals keep up with the latest discoveries as a mean to expand their knowledge and capabilities. Once the causality is placed in the medical genetics realm, there is not much a physician can actively do. Yet being informed or even warned is important. It’s the extremely serious game of medical hypotheses that just gained a new valid member.
Although unable to assist the patient into the details of medical genetics unless specialized in this particular field, any doctor might benefit from considering this type of cause for HBP. It is the collateral effect that matters. Simply by knowing there might be such a cause, the field of diagnose opens up in a different way. Perhaps new therapies based on these discoveries will also appear. They might even be accessible to any primary hypertension sufferer. Knowing more is better than not knowing enough – at least in the medical field.
How about the patients? If anything, genetics reminds the non-specialists once more that everyone is unique. What fits one individual might not fit another. Yet, due to group phenomena, there are shared predispositions, similar conditions, benefits and adverse factors when it comes to healthcare. It is therefore important to try and profile yourself correctly during medical visits. Practicing this exercise at home is also useful.
Aiming to be healthier? Observe your habits
Nobody knows yourself better than you. That is as long as you learn to know yourself. Objective awareness when it comes to our daily habits, to the changes in our routine and our state, moods and symptoms can provide an accurate image of what causes different reactions.
Of course, specialized help translates such observations into pertinent diagnosis, recommendations and suited therapy. Therefore, by joining patient forces with the physicians’ knowledge, the chances of improvement can greatly increase.