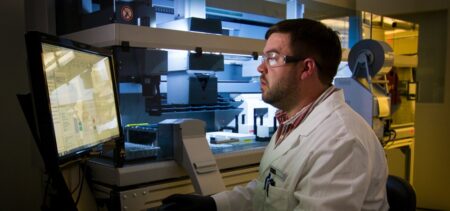
Health plans have been expanding the use of prior authorization as a tool to control costs for several years, to the frustration of physicians. MGMA members put the practice at the top of a list of burdensome issues that include COVID-19 workplace mandates, audits and lack of electronic health record interoperability, among other challenges.
The administrative hurdles require medical practices to obtain authorization before providing treatments, tests or prescription drugs to patients. Physicians say the requirements not only delay patient care but also raise provider costs, by increasing time spent by staff to secure authorizations. Those challenges have been compounded during the pandemic by staffing shortages and intense competition for workers in the tightened labor market, MGMA said.